
Chronic periodontal disease, or periodontitis, poses a significant threat to oral health, impacting the gums and supportive tissues around the teeth.
Characterized by inflammation and gradual tissue destruction, this condition can lead to tooth loss if left untreated.
Understanding its causes, symptoms, and treatment options is crucial for effective management. From plaque accumulation to genetic predisposition and systemic factors, various factors contribute to its development.
Early diagnosis through comprehensive evaluation enables timely intervention, ranging from non-surgical therapies to advanced surgical procedures.
With proper prevention strategies and proactive management, individuals can mitigate the risks associated with chronic periodontal disease and preserve their oral health for the long term.
Chronic Periodontal Disease
Chronic periodontal disease, commonly known as periodontitis, stands as a formidable adversary to oral health, silently wreaking havoc on the gums and supportive structures around the teeth.
This insidious condition, characterized by inflammation and progressive tissue degradation, poses a significant risk of tooth loss if left unchecked. Understanding its complexities, from root causes to treatment modalities, is paramount in combating its detrimental effects and preserving oral well-being.
Unraveling the Origins
At the heart of chronic periodontal disease lies a vicious cycle initiated by the accumulation of plaque, a sticky film of bacteria, and debris adhering to the tooth surfaces.
Poor oral hygiene practices, combined with factors such as smoking, genetic predisposition, systemic diseases like diabetes, hormonal fluctuations, and certain medications, create a fertile environment for periodontal inflammation to flourish.
Over time, this inflammatory cascade leads to irreversible damage to the gingival tissue, periodontal ligament, and underlying bone.
Recognizing the Telltale Signs
Identifying chronic periodontal disease in its early stages is pivotal for successful intervention. Common indicators include swollen, tender, and bleeding gums, persistent halitosis (bad breath), receding gumlines, tooth mobility, and changes in the fit of dental appliances.
While these symptoms may initially seem benign, they serve as warning signals of underlying periodontal pathology and should prompt immediate evaluation by a dental professional.
Navigating the Diagnostic Process
Diagnosing chronic periodontal disease involves a comprehensive periodontal assessment, encompassing thorough probing of gum pockets, dental X-rays to visualize bone loss, and clinical examination of soft tissue health.
This meticulous evaluation enables dental professionals to classify the severity of periodontal disease and tailor treatment plans accordingly.
Crafting an Arsenal of Treatment Modalities
Treatment of chronic periodontal disease hinges on the principles of arresting disease progression, preserving existing tooth structure, and restoring periodontal health.
Nonsurgical interventions, such as scaling and root planing (deep cleaning) to remove plaque and calculus deposits, serve as the cornerstone of periodontal therapy. Adjunctive measures, including antimicrobial agents and host modulation therapy, may be employed to enhance treatment outcomes.
In cases of advanced periodontitis, surgical interventions may be necessary to address deep gum pockets, regenerate lost bone, or recontour soft tissue defects.
Surgical procedures such as flap surgery, bone grafting, guided tissue regeneration, and gingival grafting aim to restore periodontal anatomy and promote tissue regeneration.
Embracing Preventive Strategies
Prevention lies at the forefront of managing chronic periodontal disease. Embracing meticulous oral hygiene practices, including regular brushing, flossing, and interdental cleaning, serves as the first line of defense against plaque accumulation.
Routine dental visits for professional cleanings and comprehensive examinations enable early detection of periodontal disease and timely intervention. I hope now you are aware of Chronic periodontal Disease.
What is chronic periodontal disease?
Understanding the Condition
Chronic periodontal disease, also known as periodontitis, is a pervasive oral health issue characterized by inflammation and tissue damage around the teeth.
Causes and Factors
Various factors contribute to its development, including plaque buildup, poor oral hygiene, smoking, genetic predisposition, systemic diseases, hormonal changes, and certain medications.
Symptoms and Indicators
Signs of chronic periodontal disease include swollen and bleeding gums, persistent bad breath, receding gums, tooth mobility, and changes in the fit of dental appliances.
Diagnosis and Evaluation
Diagnosis involves a comprehensive periodontal assessment, including probing of gum pockets, dental X-rays, and clinical examination to determine the severity of the disease.
Treatment Approaches
Treatment strategies range from nonsurgical therapies like scaling and root planing to surgical interventions such as flap surgery and tissue regeneration techniques in advanced cases.
Preventive Measures
Prevention focuses on maintaining good oral hygiene, regular dental visits, lifestyle modifications, and early intervention to prevent disease progression and preserve oral health.
Aggressive periodontal Disease
Overview of the Condition
Aggressive periodontal disease is a severe form of periodontitis characterized by rapid progression and pronounced tissue destruction around the teeth.
Contributing Factors
Genetic predisposition, compromised immune function, and bacterial pathogens play key roles in the development and progression of aggressive periodontal disease.
Manifestations and Symptoms
Symptoms include rapid loss of gum attachment and supporting bone, excessive tooth mobility, gum recession, and pus formation.
Diagnosis and Assessment
Diagnosis involves thorough periodontal evaluation, including probing of gum pockets, dental X-rays, and assessment of clinical signs to determine disease severity.
Treatment Approaches
Treatment typically involves aggressive management strategies, including scaling and root planing, antimicrobial therapy, and surgical interventions such as flap surgery and bone grafting.
Prognosis and Management
The prognosis depends on early detection and intervention. Long-term management focuses on meticulous oral hygiene, regular dental visits, and ongoing periodontal maintenance to prevent recurrence.
Step-by-step Guide to Treating Chronic Periodontal Disease
Step 1: Initial Assessment
Conduct a comprehensive examination, including probing of gum pockets, assessment of clinical signs, and dental X-rays to evaluate the extent of periodontal disease.
Step 2: Professional Cleaning
Initiate treatment with scaling and root planing to remove plaque, tartar, and bacteria from tooth surfaces and below the gumline, promoting gum health and reducing inflammation.
Step 3: Antibacterial Therapy
Administer antimicrobial agents, such as prescription mouth rinses or local antibiotics, to reduce bacterial load and prevent infection recurrence in periodontal pockets.
Step 4: Oral Hygiene Education
Educate the patient on proper oral hygiene practices, emphasizing the importance of daily brushing, flossing, and interdental cleaning to maintain periodontal health at home.
Step 5: Periodontal Maintenance
Schedule regular follow-up appointments for periodontal maintenance visits, during which plaque and tartar buildup are monitored and removed, and the effectiveness of home care is evaluated.
Step 6: Surgical Intervention (if necessary)
Consider surgical options, such as flap surgery or bone grafting, for advanced cases of periodontal disease to address deep gum pockets and restore damaged tissue and bone.
Step 7: Adjunctive Therapies
Explore adjunctive treatments like laser therapy or host modulation agents to enhance treatment outcomes and promote tissue healing.
Step 8: Systemic Health Management
Collaborate with other healthcare providers to manage systemic conditions that may impact periodontal health, such as diabetes or cardiovascular disease, to optimize overall health outcomes.
Step 9: Long-term Monitoring and Maintenance
Implement a long-term monitoring plan with regular dental visits for ongoing evaluation of periodontal status, reinforcement of oral hygiene practices, and adjustment of treatment as needed to ensure continued periodontal health.
Can You Fully Recover From Periodontal Disease?
While periodontal disease cannot be fully cured, it can be effectively managed and its progression halted with proper treatment and ongoing maintenance.
With timely intervention and comprehensive care, individuals can achieve significant improvement in gum health and prevent further deterioration of the periodontal tissues.
Treatment strategies for periodontal disease typically focus on removing bacterial plaque and tartar buildup from the teeth and gums, reducing inflammation, and addressing any underlying factors contributing to the disease.
This may involve professional cleanings, scaling and root planing procedures, antimicrobial therapy, and, in advanced cases, surgical interventions such as flap surgery or bone grafting.
Additionally, ongoing oral hygiene practices, including regular brushing, flossing, and interdental cleaning, along with routine dental visits for professional cleanings and check-ups, are essential for maintaining periodontal health and preventing disease recurrence.
While complete reversal of periodontal disease may not be possible, with proper management and diligent care, individuals can achieve significant improvement in gum health, prevent further damage to the periodontal tissues, and enjoy a healthy smile for years to come.
It’s important to work closely with a dental professional to develop a personalized treatment plan and adhere to recommended oral hygiene practices to optimize periodontal health.
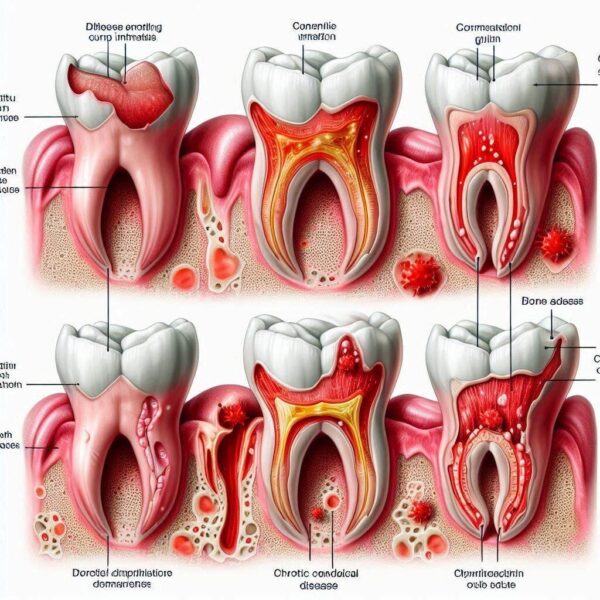
What Are The Chronic Periodontal Disease Side Effects?

Chronic periodontal disease can lead to various side effects and complications if left untreated. These may include:
Side Effects of Chronic Periodontal Disease:
1. Gum Recession:
Chronic periodontal disease can cause the gums to pull away from the teeth, leading to gum recession. This exposes the tooth roots, making them more susceptible to decay and sensitivity.
2. Tooth Mobility:
As periodontal disease progresses, the supporting bone around the teeth may deteriorate, resulting in increased tooth mobility. This can eventually lead to tooth loss if not addressed.
3. Tooth Loss:
Advanced chronic periodontal disease can cause irreversible damage to the periodontal tissues and supporting bone, ultimately resulting in tooth loss.
4. Abscess Formation:
Pockets of pus, known as abscesses, may form around the affected teeth due to bacterial infection. Abscesses can cause pain, swelling, and further tissue destruction if left untreated.
5. Halitosis (Bad Breath):
The buildup of bacteria and debris in the periodontal pockets can lead to persistent bad breath, or halitosis, which may be difficult to eliminate with regular oral hygiene practices.
6. Changes in Bite Alignment:
Severe bone loss associated with chronic periodontal disease can alter the alignment of the teeth and affect bite function, leading to difficulties in chewing and speaking.
7. Systemic Health Risks:
Chronic periodontal disease has been linked to an increased risk of various systemic health conditions, including cardiovascular disease, diabetes, respiratory infections, and adverse pregnancy outcomes.
8. Aesthetic Concerns:
Gum recession, tooth mobility, and tooth loss can impact the aesthetics of the smile, leading to self-consciousness and a reduced quality of life.
How Can I Fix My Periodontal Disease Naturally?

While natural remedies can complement professional treatment for periodontal disease, they are not a substitute for professional dental care.
However, incorporating certain practices into your oral hygiene routine may help support gum health and manage symptoms. Here are some natural approaches to consider:
Natural Remedies for Periodontal Disease:
1. Proper Oral Hygiene:
Brush your teeth twice daily with a soft-bristled toothbrush and fluoride toothpaste. Floss or use interdental brushes daily to clean between teeth and along the gumline.
2. Saltwater Rinse:
Rinse your mouth with warm salt water to reduce inflammation and bacteria. Mix one teaspoon of salt in a glass of warm water and swish it around your mouth for about 30 seconds before spitting it out.
3. Oil Pulling:
Swishing coconut oil or sesame oil in your mouth for about 15-20 minutes may help reduce plaque and bacteria. Spit out the oil and rinse your mouth thoroughly with water afterward.
4. Herbal Mouthwashes:
Certain herbal mouthwashes containing ingredients like tea tree oil, peppermint oil, or sage extract may help reduce inflammation and bacterial growth. Use as directed by the manufacturer.
5. Aloe Vera Gel:
Apply a small amount of pure aloe vera gel to your gums to soothe inflammation and promote healing. Ensure the gel is free from added sugars or flavorings.
6. Green Tea:
Drink green tea regularly, as it contains antioxidants that may help reduce inflammation and support gum health. Opt for unsweetened varieties for maximum benefit.
7. Probiotics:
Consuming probiotic-rich foods like yogurt, kefir, or sauerkraut may help balance oral microbiota and reduce the risk of periodontal disease.
8. Stress Reduction:
Manage stress through relaxation techniques such as deep breathing, meditation, yoga, or regular exercise. Chronic stress can weaken the immune system and exacerbate gum inflammation.
9. Balanced Diet:
Maintain a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Avoid sugary and processed foods, which can contribute to bacterial growth and inflammation.
Can Periodontal Disease Be Cured Without Surgery?

While periodontal disease cannot be “cured” in the traditional sense without professional intervention, its progression can often be halted and managed effectively without surgery, especially in its early stages.
Non-surgical treatments can address the underlying causes of periodontal disease and promote gum health. These treatments may include:
Non-Surgical Treatments for Periodontal Disease:
1. Professional Cleaning:
Scaling and root planing (deep cleaning) performed by a dental hygienist or dentist can remove plaque, tartar, and bacterial toxins from the tooth surfaces and below the gumline, promoting gum health and reducing inflammation.
2. Antibacterial Therapy:
Topical or systemic antibiotics may be prescribed to reduce bacterial load and inhibit bacterial growth in periodontal pockets, helping to control infection and inflammation.
3. Antimicrobial Mouth Rinses:
Prescription mouth rinses containing antimicrobial agents may be recommended to reduce plaque accumulation and bacterial growth, promoting periodontal health.
4. Maintenance Therapy:
Regular follow-up appointments for periodontal maintenance visits are essential for monitoring gum health, removing plaque and tartar buildup, and assessing the effectiveness of home care.
5. Oral Hygiene Education:
Education on proper oral hygiene practices, including brushing, flossing, and interdental cleaning techniques, helps empower patients to maintain optimal oral health at home.
6. Adjunctive Therapies:
Additional treatments such as laser therapy, photodynamic therapy, or local antimicrobial agents may be used to enhance treatment outcomes and promote tissue healing.
7. Lifestyle Modifications:
Lifestyle factors such as smoking cessation, stress management, and maintaining a balanced diet can play a significant role in managing periodontal disease and supporting gum health.
Conclusion:
Chronic periodontal disease is a formidable adversary, capable of inflicting irreversible damage if left unchecked.
However, armed with knowledge and armed with knowledge and equipped with proactive preventive measures, individuals can thwart its progression and safeguard their oral health.
By fostering a collaborative partnership with dental professionals and embracing a culture of preventive care, we can pave the path toward optimal periodontal health and preserve the longevity of our smiles for years to come. I hope that after reading the entire article you are fully aware of everything about Chronic periodontal Disease.
FAQs: Chronic Periodontal Disease
Q1: What is chronic periodontal disease?
A1: Chronic periodontal disease, also known as periodontitis, is a progressive inflammatory condition that affects the gums and supporting structures of the teeth. It is characterized by the gradual destruction of the gingival tissue, periodontal ligament, and alveolar bone.
Q2: What causes chronic periodontal disease?
A2: Chronic periodontal disease is primarily caused by the accumulation of plaque, a sticky film of bacteria and food debris, on the teeth and along the gumline. Other contributing factors include poor oral hygiene, smoking, genetic predisposition, systemic diseases (such as diabetes), hormonal changes, and certain medications.
Q3: What are the symptoms of chronic periodontal disease?
A3: Symptoms of chronic periodontal disease may include swollen, red, and bleeding gums, persistent bad breath, receding gums, loose or shifting teeth, and changes in the fit of dentures or other dental appliances.
Q4: Can chronic periodontal disease be cured?
A4: While chronic periodontal disease cannot be fully cured, its progression can be effectively managed and its symptoms controlled with proper treatment. Early detection and intervention are crucial for preventing further damage to the periodontal tissues and preserving oral health.
Q5: What are the treatment options for chronic periodontal disease?
A5: Treatment options for chronic periodontal disease include professional cleanings (scaling and root planing), antimicrobial therapy, oral hygiene education, surgical interventions (if necessary), and lifestyle modifications. The most appropriate treatment approach depends on the severity of the disease and individual patient factors.
