
A tooth infection, or dental abscess, is a serious dental condition that occurs when bacteria invade the dental pulp—the innermost part of the tooth containing nerves and blood vessels.
This can lead to severe pain, swelling, and other complications if left untreated. Recognizing the early signs of a tooth infection, such as persistent toothache, sensitivity to hot or cold, swelling, and a bad taste in the mouth, is crucial for timely intervention.
Prompt dental care is essential to prevent the infection from spreading and to address the underlying issue effectively, ensuring overall oral health and well-being.
How Do You Know If You Have Tooth Infection

A tooth infection, also known as a dental abscess, can cause various symptoms that indicate an issue requiring prompt dental attention. Recognizing these signs early can help you seek treatment before the infection spreads or worsens. Here are common indicators of a tooth infection:
Pain and Sensitivity
- Persistent Toothache: A continuous, throbbing pain in the affected tooth or surrounding area is a common symptom. The pain may worsen when lying down or with exposure to hot, cold, or sweet foods and drinks.
- Sensitivity: Increased sensitivity to temperature changes and pressure can signal an infection.
Swelling and Redness
- Gum Swelling: Swelling around the infected tooth and gums is typical. The area might feel tender and appear red or inflamed.
- Facial Swelling: In severe cases, the infection can cause swelling in the face, jaw, or neck, indicating that the infection has spread.
Bad Taste and Odor
- Bad Taste in Mouth: An unpleasant taste in your mouth can occur if the abscess ruptures, releasing pus.
- Bad Breath: Persistent bad breath, despite good oral hygiene, can be a sign of an infection.
Fever and Malaise
- Fever: A fever may develop as your body tries to fight the infection.
- General Malaise: Feeling generally unwell, fatigued, or having a low energy level can accompany a tooth infection.
Pus and Drainage
- Pus Formation: The presence of pus, which may drain from the infected area, is a clear sign of an abscess. This pus is typically yellowish or greenish in color.
- Drainage: If the abscess bursts, you might notice a sudden rush of foul-tasting fluid in your mouth.
Difficulty Chewing and Swallowing
- Pain While Chewing: Chewing can become painful due to the pressure on the infected tooth.
- Difficulty Swallowing: Swelling and infection can make it hard to swallow or open your mouth fully.
When to Seek Medical Attention
If you experience any of the above symptoms, it’s crucial to see a dentist as soon as possible. A tooth infection can spread to other parts of the body, leading to more serious health complications if left untreated.
Diagnosis and Treatment
- Dental Examination: Your dentist will examine the affected tooth and surrounding area, possibly taking x-rays to determine the extent of the infection.
- Treatment Options: Treatment may include draining the abscess, prescribing antibiotics to clear the infection, and performing procedures like a root canal or tooth extraction to remove the source of the infection.
What Is Tooth Infection
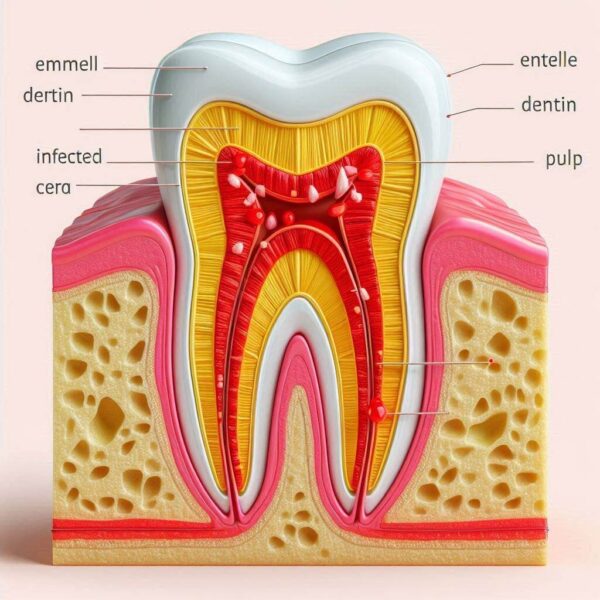
A tooth infection, also known as a dental abscess, occurs when bacteria invade the innermost part of the tooth, called the dental pulp. The dental pulp contains nerves, blood vessels, and connective tissue, and when it becomes infected, it can lead to significant pain and discomfort. There are two main types of dental abscesses:
Types of Dental Abscesses
- Periapical Abscess: This type of abscess occurs at the tip of the tooth’s root. It usually starts from a bacterial infection that has spread from the tooth’s pulp, often due to untreated tooth decay or a traumatic injury to the tooth.
- Periodontal Abscess: This abscess occurs in the gums at the side of the tooth root. It typically develops due to severe gum disease (periodontitis), which causes the gums to pull away from the teeth, creating pockets that can become infected.
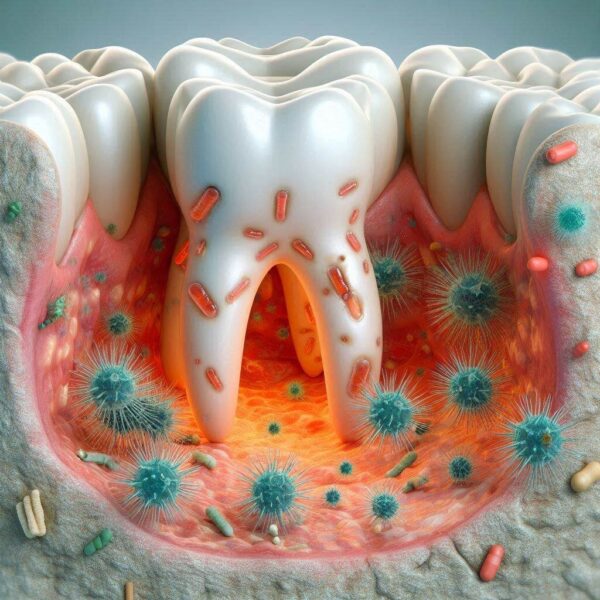
Causes of Tooth Infection
- Tooth Decay: Untreated cavities can allow bacteria to reach the dental pulp, leading to an infection.
- Gum Disease: Advanced gum disease can create pockets around the teeth that harbor bacteria, leading to an infection.
- Trauma: A cracked or chipped tooth can provide an entry point for bacteria.
- Previous Dental Work: Sometimes, dental procedures that expose the pulp can lead to infections if bacteria infiltrate.
Symptoms of Tooth Infection
- Severe Toothache: Persistent, throbbing pain that can radiate to the jawbone, neck, or ear.
- Swelling: Swelling in the face, cheek, or neck.
- Sensitivity: Increased sensitivity to hot, cold, or pressure.
- Fever: A high temperature can indicate the body is fighting an infection.
- Bad Taste and Odor: A bad taste in the mouth and foul-smelling breath.
- Pus: Presence of pus or drainage in the mouth.
- Difficulty Chewing and Swallowing: Pain while chewing and difficulty opening the mouth.
Diagnosis and Treatment
- Dental Examination: Dentists use visual examination and x-rays to diagnose the extent of the infection.
- Treatment: Treatment options include draining the abscess, antibiotics to clear the infection, root canal therapy to remove the infected pulp, or tooth extraction if the tooth is severely damaged.
How To Treat Tooth Infection?

Treating a tooth infection, or dental abscess, involves addressing both the infection and the underlying cause to prevent recurrence.
The first step is to see a dentist as soon as possible if you suspect a tooth infection. Delaying treatment can lead to more serious complications, including the spread of the infection to other parts of the body.
Diagnosis
Your dentist will conduct a thorough examination, which may include a visual examination to check for signs of infection, such as swelling, redness, and pus. X-rays might be taken to determine the extent of the infection and to identify any damage to the tooth, surrounding bone, or neighboring teeth.
Drainage of the Abscess
To relieve pain and eliminate the pus, your dentist may need to drain the abscess. This procedure involves making a small incision in the abscess to allow the pus to escape. In some cases, a small drain may be placed to keep the area open and allow for continued drainage.
Antibiotics
If the infection has spread or if you have a weakened immune system, your dentist may prescribe antibiotics to help eliminate the bacterial infection. Common antibiotics for dental infections include amoxicillin, clindamycin, and metronidazole.
Root Canal Therapy
If the tooth is salvageable, root canal therapy may be recommended. This procedure involves removing the infected pulp, cleaning out the root canals, and then filling and sealing them to prevent reinfection. The tooth may then be restored with a crown or filling to return it to full function and appearance.
Tooth Extraction
If the tooth is severely damaged and cannot be saved, extraction may be necessary. This involves removing the infected tooth to prevent the spread of infection. After extraction, it’s important to follow your dentist’s instructions for aftercare, including managing pain and preventing infection at the extraction site.
Pain Management
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain and reduce inflammation. Your dentist may also recommend specific pain management strategies.
Follow-Up Care
Regular follow-up appointments with your dentist are important to ensure that the infection is completely resolved and that there are no complications. Your dentist will also check the healing progress and the effectiveness of the treatment provided.
Preventive Measures
To prevent future tooth infections, maintain good oral hygiene by brushing and flossing regularly, visit your dentist for regular check-ups and cleanings, and treat dental issues like cavities and gum disease promptly. Using a mouthguard if you play contact sports can help prevent trauma to your teeth.
Does Tooth Infection Go Away Normally

A tooth infection, also known as a dental abscess, does not go away on its own and requires professional treatment. Dental abscesses can lead to serious health complications if left untreated. Understanding the importance of seeking prompt dental care is crucial to prevent further issues.
Why a Tooth Infection Needs Treatment
Tooth infections occur when bacteria invade the dental pulp, the innermost part of the tooth containing nerves and blood vessels. The body’s immune system cannot easily reach and eliminate bacteria within the tooth structure, making professional intervention necessary.
Without treatment, the infection can spread to surrounding tissues, including the jawbone, neck, and other parts of the body.
Spread of Infection
The infection can spread to other parts of the body, leading to potentially life-threatening conditions like sepsis, a systemic infection that can cause organ failure.
Bone Loss
Untreated infections can lead to the destruction of bone around the tooth, causing tooth loss and requiring more complex dental procedures.
Chronic Pain
Persistent and severe pain is common with tooth infections, significantly impacting daily activities and overall quality of life.
Facial Swelling
The infection can cause noticeable swelling in the face, cheek, or neck, interfering with breathing and swallowing.
Abscess Formation
The accumulation of pus can lead to abscesses that may rupture, causing further complications and severe pain.
Treatment Options
Professional dental treatment is essential for resolving a tooth infection. Common treatments include:
Antibiotics
Prescribed to control and eliminate the bacterial infection, particularly if it has spread beyond the tooth.
Drainage
Draining the abscess to remove pus and reduce pressure and pain.
Root Canal Therapy
Removing the infected pulp, cleaning the root canals, and sealing the tooth to prevent reinfection.
Tooth Extraction
Removing the infected tooth if it cannot be saved, followed by appropriate aftercare to prevent complications.
Preventive Measures
To reduce the risk of tooth infections, maintain good oral hygiene by brushing and flossing daily, visit your dentist regularly for check-ups and cleanings, and address dental issues promptly. Avoiding sugary foods and drinks and using protective gear during contact sports can also help prevent damage to teeth.
What Does An Infection In Your Tooth Feel Like?

A tooth infection, also known as a dental abscess, can cause various symptoms that indicate an issue requiring prompt dental attention. Recognizing these signs early can help you seek treatment before the infection spreads or worsens. Here’s what an infection in your tooth may feel like:
Persistent Toothache
One of the most common symptoms of a tooth infection is a persistent and throbbing toothache. The pain may be localized to the affected tooth but can also radiate to the jawbone, ear, or neck. The intensity of the pain may increase when biting down or applying pressure on the tooth.
Sensitivity to Temperature Changes
You may experience increased sensitivity to hot or cold temperatures, especially when consuming hot or cold foods and beverages. The sensitivity may linger even after the stimulus is removed.
Swelling and Redness
Swelling around the affected tooth and gums is typical with a tooth infection. The area may appear red or inflamed and feel tender to the touch. In severe cases, the swelling may extend to the face, cheek, or neck.
Pus or Abscess Formation
The presence of pus or an abscess near the affected tooth is a clear sign of an infection. Pus may drain from the abscess, causing a foul taste in the mouth and bad breath. Abscesses can form on the gums, between teeth, or at the tip of the tooth’s root.
Difficulty Chewing and Swallowing
Pain while chewing or difficulty swallowing may occur due to pressure and inflammation around the infected tooth. You may also experience difficulty opening your mouth fully.
Fever and General Malaise
In some cases, a tooth infection can lead to a fever as your body’s immune system responds to the infection. General malaise, including fatigue, aches, and a feeling of being unwell, may also accompany the fever.
Bad Taste and Odor
An unpleasant taste in your mouth, despite good oral hygiene practices, can indicate the presence of pus or drainage from the infected tooth. Foul-smelling breath (halitosis) may also occur due to the presence of bacteria and decaying tissue.
What Is The First Stage Of Tooth Infection?
The First Stage of Tooth Infection: Early Signs and Symptoms
The first stage of a tooth infection, also known as a dental abscess, often begins with subtle signs that may go unnoticed until the infection progresses. Recognizing these early symptoms is crucial for seeking prompt dental care and preventing the infection from worsening. Here’s what to look out for in the first stage of a tooth infection:
1. Sensitivity to Hot or Cold
One of the earliest signs of a tooth infection is increased sensitivity to hot or cold temperatures, particularly when consuming food or beverages. You may notice discomfort or pain that lingers even after removing the stimulus.
2. Mild Discomfort or Toothache
At the onset of a tooth infection, you may experience mild discomfort or occasional toothache in the affected tooth. The pain may be intermittent and not severe enough to disrupt daily activities.
3. Gum Sensitivity and Swelling
The gums around the affected tooth may become tender and slightly swollen. You may notice mild inflammation or redness in the gum tissue near the tooth.
4. Bad Taste or Breath
As the infection progresses, you may experience a persistent bad taste in your mouth or foul-smelling breath (halitosis). This can occur due to the presence of bacteria and decay within the tooth or surrounding tissues.
5. Prolonged Tooth Sensitivity
If left untreated, the sensitivity of the tooth to hot, cold, or pressure may become more persistent and pronounced. You may find it increasingly uncomfortable to eat or drink certain foods.
6. Discoloration of the Tooth
In some cases, the infected tooth may develop discoloration, appearing darker or greyish in color compared to surrounding teeth. This discoloration can indicate damage to the tooth pulp caused by the infection.
Does Tooth Infection Affect Entire Body
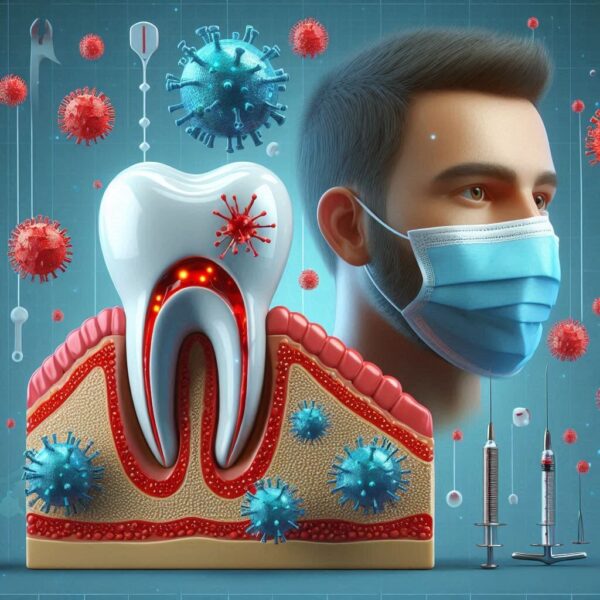
A tooth infection, if left untreated, can potentially affect the entire body and lead to serious health complications.
While the initial focus of a tooth infection is localized to the oral cavity, the infection can spread to other parts of the body through the bloodstream or by direct extension. Here’s how a tooth infection can impact the entire body:
Spread of Infection
- Sepsis: In severe cases, bacteria from a tooth infection can enter the bloodstream and cause sepsis, a life-threatening condition characterized by a systemic inflammatory response. Sepsis can lead to organ failure and death if not treated promptly.
- Endocarditis: Bacteria from a tooth infection can travel to the heart and cause endocarditis, an infection of the inner lining of the heart chambers and valves. Endocarditis can damage the heart valves and lead to heart failure or stroke.
- Brain Abscess: In rare cases, bacteria can travel to the brain and cause a brain abscess, a collection of pus within the brain tissue. Brain abscesses can cause neurological symptoms such as headaches, seizures, and altered mental status.
Impact on Overall Health
- Immune System Response: Chronic dental infections can put stress on the immune system, making it less effective at fighting off other infections and diseases.
- Inflammation: The body’s inflammatory response to a tooth infection can contribute to systemic inflammation, which has been linked to various chronic health conditions such as heart disease, diabetes, and rheumatoid arthritis.
Oral-Systemic Link
Research has shown a strong association between oral health and overall health, highlighting the importance of maintaining good oral hygiene and seeking prompt dental care for dental infections.
Poor oral health has been linked to an increased risk of systemic diseases, including cardiovascular disease, diabetes, respiratory infections, and adverse pregnancy outcomes. I hope after reading so far you can understand the importance of the question How Do You Know If You Have Tooth Infection.
What Are The Side Effects Of Tooth Infection

Side Effects of Tooth Infection
A tooth infection, if left untreated, can lead to various side effects and complications that affect both oral health and overall well-being. Understanding these potential consequences is crucial for recognizing the importance of seeking timely dental care. Here are the common side effects of a tooth infection:
1. Persistent Pain
The most noticeable side effect of a tooth infection is persistent and often severe pain in the affected tooth or surrounding area. The pain may worsen with biting, chewing, or applying pressure on the tooth.
2. Swelling and Inflammation
Swelling and inflammation are common side effects of a tooth infection. The gums around the infected tooth may become swollen, red, and tender to the touch. In severe cases, facial swelling may occur, affecting the cheeks, jaw, or neck.
3. Pus or Abscess Formation
The accumulation of pus within the tooth or surrounding tissues can lead to the formation of an abscess. Abscesses are pockets of infection that may appear as swollen, painful bumps on the gums or as localized areas of swelling and tenderness.
4. Bad Taste and Breath
The presence of pus and bacterial infection can result in a foul taste in the mouth and persistent bad breath (halitosis). Despite maintaining good oral hygiene, the bad taste and odor may persist until the infection is resolved.
5. Fever and Malaise
As the body’s immune system responds to the infection, fever and general malaise may develop. Fever is the body’s natural response to infection, while malaise refers to a general feeling of discomfort, fatigue, and overall unwellness.
6. Difficulty Eating and Speaking
Pain, swelling, and discomfort associated with a tooth infection can make it difficult to eat, chew, or speak comfortably. You may experience pain or sensitivity when biting down or moving your jaw, leading to dietary changes and speech difficulties.
7. Spread of Infection
If left untreated, a tooth infection can spread to other parts of the body, leading to systemic complications such as sepsis, endocarditis, or brain abscess. These serious conditions can be life-threatening and require immediate medical attention.
8. Tooth Mobility and Loss
In advanced cases of tooth infection, the surrounding bone and supporting structures may be damaged, leading to tooth mobility or loosening. Without intervention, the tooth may eventually become irreversibly damaged and require extraction.
How to Know if You Have a Tooth Infection: Conclusion
Recognizing the signs and symptoms of a tooth infection is vital for prompt treatment and preventing complications.
Common indicators include persistent toothache, sensitivity to hot or cold, swelling, bad taste or breath, and fever. Difficulty chewing or speaking and the presence of pus or abscesses may also signal an infection.
Consulting a dentist promptly upon experiencing these symptoms is crucial to prevent the infection from spreading and causing further harm. I hope now you are fully aware of How Do You Know If You Have Tooth Infection.
Frequently Asked Questions (FAQs)
Q1. Can a tooth infection go away on its own?
A1. A tooth infection typically does not resolve without treatment and may worsen over time. Professional dental care is necessary to effectively address the infection.
Q2. What happens if you ignore a tooth infection?
A2. Ignoring a tooth infection can lead to severe pain, abscess formation, bone loss, and potentially life-threatening complications if the infection spreads to other parts of the body.
Q3. How is a tooth infection diagnosed?
A3. A dentist can diagnose a tooth infection through a combination of visual examination, dental X-rays, and assessment of symptoms such as pain, swelling, and sensitivity.
Q4. What is the treatment for a tooth infection?
A4. Treatment options for a tooth infection may include antibiotics to control the infection, root canal therapy to remove infected pulp, or tooth extraction for severe cases. Drainage of abscesses may also be necessary.
Q5. How can tooth infections be prevented?
A5. Maintaining good oral hygiene practices, visiting the dentist regularly for check-ups and cleanings, addressing dental issues promptly, and avoiding sugary foods and drinks can help prevent tooth infections.
