
Accidents happen, and occasionally, we find ourselves in situations where we inadvertently bump or hit our heads. While most of the time these incidents result in little more than a temporary discomfort, there are instances when individuals may notice a small dent or indentation in their forehead following such an event. This occurrence can be concerning and may prompt questions about the underlying cause and potential implications for one’s health.
In this article, we’ll explore the phenomenon of developing a small dent in the forehead after hitting the head, shedding light on the possible reasons behind it and addressing common concerns. By understanding “Small Dent In Forehead After Hitting Head” and the factors at play and seeking appropriate medical guidance, individuals can gain clarity and peace of mind regarding this seemingly minor yet potentially worrisome issue.
Small Dent In Forehead After Hitting Head
Detail Guide:
1. Subcutaneous Tissue Injury:
One possible explanation for a small dent in the forehead after hitting the head is the formation of a subcutaneous hematoma or soft tissue injury. When the head sustains trauma, the underlying blood vessels and tissues may be damaged, leading to the accumulation of blood or fluid beneath the skin’s surface.
Over time, as the body heals, this may result in the formation of a small indentation or depression in the affected area.
2. Bone Contusion or Fracture:
In some cases, a dent in the forehead may be indicative of a bone contusion or fracture resulting from the impact of the head injury. When the force of the injury is sufficient to cause damage to the underlying skull bone, it can lead to a visible indentation or depression in the overlying skin.
It’s essential to seek medical evaluation if there is any suspicion of a skull fracture, as this may require further assessment and treatment.
3. Localized Tissue Swelling:
Following a head injury, localized tissue swelling or edema may develop in the affected area. This swelling can distort the normal contours of the forehead, resulting in the appearance of a small dent or indentation. While the swelling typically resolves on its own over time, it’s essential to monitor for any concerning symptoms and seek medical attention if necessary.
4. Scar Tissue Formation:
In some cases, the healing process following a head injury may result in the formation of scar tissue beneath the skin’s surface. This scar tissue may contract or pull on the surrounding skin, leading to the development of a small dent or depression in the forehead.
While scar tissue is a natural part of the healing process, it’s essential to monitor for any changes or complications and consult with a healthcare provider if needed.
5. Underlying Cranial Anatomy:
It’s important to recognize that the human skull is not perfectly smooth and may exhibit variations in shape and contour among individuals. A small dent or indentation in the forehead may represent a normal anatomical variation rather than a consequence of a recent head injury.
However, if the dent is new or accompanied by other concerning symptoms, it’s advisable to seek medical evaluation to rule out any underlying issues. I hope you are fully aware of “Small Dent In Forehead After Hitting Head”.
What Can Cause A Dent In The Forehead?
The human body is a complex and remarkable entity, but it’s not immune to bumps, bruises, and occasional mishaps. Sometimes, seemingly minor incidents can lead to unexpected outcomes, such as the development of a dent or indentation in the forehead.
While this phenomenon may raise concerns and prompt questions about its underlying cause and potential implications, understanding the factors at play can provide clarity and peace of mind.
In this article, we’ll explore the various factors that can cause a dent in the forehead, ranging from traumatic injuries to congenital anomalies and medical conditions. By shedding light on the possible reasons behind this occurrence and addressing common concerns, we aim to empower individuals to navigate their health with knowledge and understanding.
Cause Of Dent In The Forehead:
1. Traumatic Injury:
One of the most common causes of a dent in the forehead is a traumatic injury, such as a fall, sports-related accident, or motor vehicle collision. The force of impact can damage the underlying bone and soft tissues, leading to the formation of an indentation or depression in the forehead.
2. Skull Fracture:
A severe head injury, particularly one involving the forehead region, may result in a skull fracture. When the skull bone is fractured or depressed, it can cause a visible dent or irregularity in the forehead’s surface. Skull fractures require prompt medical evaluation and treatment to prevent complications.
3. Soft Tissue Swelling:
Following a head injury or trauma, localized swelling or edema may develop in the affected area. This swelling can distort the normal contours of the forehead, resulting in the appearance of a temporary dent or indentation. As the swelling resolves, the forehead’s appearance typically returns to normal.
4. Congenital Anomalies:
In some cases, a dent in the forehead may be present from birth due to congenital anomalies or developmental abnormalities of the skull bone. These anomalies may include conditions such as craniosynostosis, where the bones of the skull fuse prematurely, leading to skull deformities and dents.
5. Surgical Intervention:
Certain surgical procedures performed on the skull or forehead region, such as craniofacial surgeries or tumor removals, may result in the formation of a dent or irregularity in the forehead’s surface. This is often a planned outcome of the surgery and may be necessary to address underlying medical issues.
6. Inflammatory Conditions:
Inflammatory conditions affecting the forehead region, such as dermatitis, acne, or cysts, may lead to localized tissue damage or scarring. Over time, this tissue damage can result in the formation of an indentation or depression in the forehead.
7. Genetic Factors:
In some cases, genetic factors may predispose individuals to develop dents or irregularities in the forehead. These genetic variations may affect the growth and development of the skull bone, leading to structural abnormalities that manifest as dents or indentations.
8. Age-Related Changes:
As individuals age, changes in bone density and tissue elasticity may occur, resulting in alterations in the facial contour, including the forehead region. While age-related changes are typically gradual, they may contribute to the development of dents or depressions in the forehead over time.
Gorham’s Disease
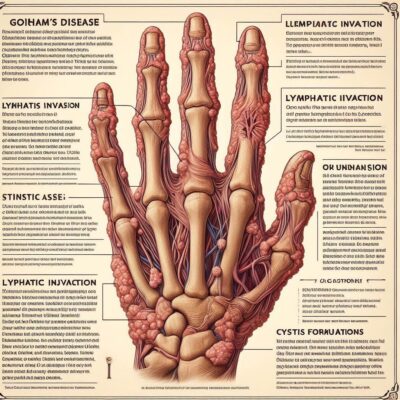
Gorham’s Disease, though rare, is a condition that can have profound effects on those diagnosed with it. Also known as Gorham-Stout disease or vanishing bone disease, it’s characterized by the progressive loss of bone tissue, leading to skeletal abnormalities and potentially debilitating complications.
Despite its rarity and enigmatic nature, understanding Gorham’s Disease is crucial for healthcare professionals and individuals alike, as early detection and management can significantly impact outcomes.
In this article, we’ll delve into Gorham’s Disease, exploring its causes, symptoms, diagnosis, and treatment options. By shedding light on this complex condition, we aim to raise awareness, provide valuable insights, and offer support to those affected by Gorham’s Disease and their caregivers.
Diseases:
1. Overview:
Gorham’s Disease is a rare disorder characterized by the spontaneous and progressive resorption of bone tissue. It primarily affects the skeletal system, leading to bone loss, structural deformities, and, in severe cases, functional impairment.
2. Causes:
The exact cause of Gorham’s Disease remains unknown. Some theories suggest that it may result from abnormalities in the lymphatic or vascular systems, leading to abnormal bone remodeling and resorption. Genetic factors may also play a role in predisposing individuals to the condition.
3. Symptoms:
The symptoms of Gorham’s Disease can vary widely depending on the location and extent of bone involvement. Common symptoms may include localized pain, swelling, weakness, fractures, and functional limitations. In some cases, Gorham’s Disease may also affect other organs or tissues, leading to additional complications.
4. Diagnosis:
Diagnosing Gorham’s Disease can be challenging due to its rarity and variable presentation. Healthcare providers typically rely on a combination of clinical evaluation, imaging studies (such as X-rays, CT scans, or MRI), and histological analysis of affected tissues to confirm the diagnosis and rule out other conditions.
5. Treatment Options:
Treatment for Gorham’s Disease aims to manage symptoms, prevent complications, and preserve function. There is no standard treatment protocol due to the rarity of the condition and limited research evidence.
Treatment options may include medication (such as bisphosphonates or calcitonin), surgical interventions (such as bone grafting or stabilization), radiation therapy, or supportive measures to address pain and functional limitations.
6. Prognosis:
The prognosis for individuals with Gorham’s Disease can vary widely depending on factors such as the extent of bone involvement, the presence of complications, and the response to treatment. In some cases, the disease may stabilize or regress spontaneously, while in others, it may progress relentlessly, leading to significant disability or even death.
7. Quality of Life:
Living with Gorham’s Disease can have a profound impact on an individual’s quality of life. Chronic pain, physical limitations, and emotional challenges may affect daily activities, relationships, and overall well-being.
It’s essential for individuals with Gorham’s Disease to receive comprehensive care and support from a multidisciplinary team, including healthcare providers, therapists, and support groups.
8. Research and Advocacy:
Due to the rarity of Gorham’s Disease, research into its underlying mechanisms, optimal treatment approaches, and long-term outcomes remain limited. Advocacy organizations and patient support groups play a crucial role in raising awareness, funding research initiatives, and providing resources and support to individuals and families affected by Gorham’s Disease.
Congenital Skull Indentation
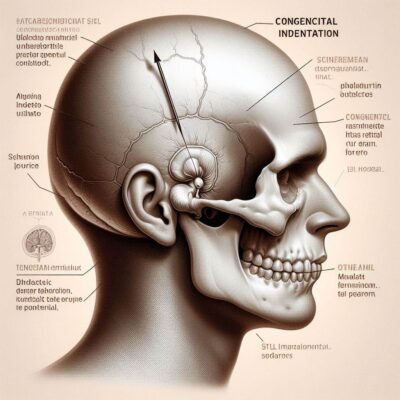
The human skull is a remarkable structure, providing protection for the brain and supporting various sensory functions. However, it’s not uncommon for individuals to notice anomalies or irregularities in the shape of their skulls, including indentations or depressions.
One such condition is congenital skull indentation, where a person is born with a noticeable depression in the skull’s surface. While congenital skull indentations may raise concerns for some individuals, understanding the factors contributing to this condition is essential for dispelling misconceptions and providing reassurance.
In this article, we’ll explore congenital skull indentation, examining its possible causes, characteristics, and implications. By shedding light on this topic, we aim to offer valuable insights and support to individuals and families who may be affected by congenital skull indentations, as well as healthcare professionals seeking to better understand this condition.
Skull Indentation:
1. Overview:
Congenital skull indentation refers to a depression or concavity in the skull that is present at birth. These indentations may vary in size, shape, and location, and they can occur as isolated anomalies or in association with other congenital conditions.
2. Causes:
The exact cause of congenital skull indentation is often unclear. In some cases, it may result from variations in fetal development, including abnormal ossification (bone formation) or pressure exerted on the skull in utero. Genetic factors may also play a role in predisposing individuals to this condition.
3. Characteristics:
Congenital skull indentations may manifest as shallow or deep depressions in the skull’s surface, typically located in the frontal, parietal, or occipital regions. These indentations may be symmetrical or asymmetrical and may or may not be associated with other physical features or developmental anomalies.
4. Diagnosis:
Congenital skull indentations are typically diagnosed during infancy or early childhood during routine physical examinations or imaging studies (such as X-rays or CT scans). Healthcare providers may evaluate the indentation’s size, location, and characteristics to determine the appropriate course of action and rule out underlying conditions.
5. Implications:
In most cases, congenital skull indentations are benign and asymptomatic, requiring no specific treatment or intervention. However, individuals with noticeable indentations may experience concerns about their appearance or potential implications for their health.
It’s essential for healthcare providers to provide reassurance and address any questions or concerns raised by patients or caregivers.
6. Treatment Options:
Treatment for congenital skull indentation is typically conservative and may focus on supportive measures such as monitoring for changes over time, providing reassurance to individuals and families, and addressing cosmetic concerns if desired.
In rare cases where the indentation is associated with underlying structural abnormalities or developmental issues, further evaluation and management may be necessary.
7. Prognosis:
The prognosis for individuals with congenital skull indentation is generally favorable, with most cases being benign and not associated with significant health problems or complications. With appropriate medical evaluation and support, individuals with congenital skull indentations can lead healthy and fulfilling lives.
8. Educational Resources and Support:
Individuals and families affected by congenital skull indentations may benefit from accessing educational resources and support networks to learn more about the condition, connect with others facing similar experiences, and access guidance and support from healthcare professionals.
Vitamin A Overdose

Vitamins are essential nutrients that play a crucial role in maintaining overall health and well-being. Among them, vitamin A is renowned for its role in supporting vision, immune function, and cell growth. However, like any other nutrient, consuming excessive amounts of vitamin A can lead to adverse effects and potentially harmful consequences.
Vitamin A overdose, though relatively rare, is a serious concern that can result in a range of symptoms and complications. Understanding the risks associated with vitamin A overdose is essential for individuals seeking to maintain a balanced and healthy diet.
In this article, we’ll explore the topic of vitamin A overdose, examining its causes, symptoms, and potential implications for health. By shedding light on this important issue, we aim to raise awareness and empower individuals to make informed choices about their dietary habits and vitamin supplementation practices.
Overdose:
1. Overview:
Vitamin A overdose, also known as hypervitaminosis A, occurs when an individual consumes excessive amounts of vitamin A, either through dietary sources or supplements. This condition can lead to toxic effects on various organ systems in the body and may have serious health consequences if left untreated.
2. Causes:
Vitamin A overdose can occur as a result of consuming high-dose vitamin A supplements, often in the form of retinol or retinyl esters. It can also result from chronic overconsumption of foods rich in preformed vitamin A, such as liver, fish liver oil, and fortified dairy products.
Additionally, certain prescription medications or skincare products containing retinoids may contribute to vitamin A toxicity if used improperly.
3. Symptoms:
The symptoms of vitamin A overdose can vary depending on the severity of the condition and the duration of exposure to high levels of vitamin A. Common symptoms may include nausea, vomiting, headache, dizziness, fatigue, and irritability. In more severe cases, individuals may experience symptoms such as blurred vision, bone pain, hair loss, skin changes, and liver damage.
4. Diagnosis:
Diagnosing vitamin A overdose typically involves a thorough medical history review, physical examination, and laboratory tests to assess vitamin A levels in the blood. Imaging studies, such as X-rays or bone scans, may also be used to evaluate for signs of bone abnormalities or other complications associated with vitamin A toxicity.
5. Treatment:
Treatment for vitamin A overdose focuses on discontinuing vitamin A supplementation and addressing symptoms and complications as needed. In mild cases, symptoms may resolve on their own once vitamin A intake is reduced. In more severe cases, supportive measures such as intravenous fluids, antiemetics, and monitoring of liver function may be necessary.
6. Prevention:
Preventing vitamin A overdose involves maintaining a balanced and varied diet that includes sources of vitamin A from both plant-based (provitamin A carotenoids) and animal-based (preformed vitamin A) sources. It’s essential to avoid excessive supplementation with high-dose vitamin A supplements unless prescribed by a healthcare provider.
Individuals should also use caution when using skincare products or medications containing retinoids and follow usage instructions carefully.
7. Risks and Complications:
Vitamin A overdose can have serious health consequences, particularly if left untreated or if high levels of vitamin A are sustained over time. Potential complications may include liver damage, bone abnormalities, increased intracranial pressure, and birth defects if vitamin A toxicity occurs during pregnancy.
8. Seeking Medical Advice:
If you suspect that you or someone else may be experiencing vitamin A overdose, it’s essential to seek medical advice promptly. Healthcare providers can conduct a thorough evaluation, provide appropriate treatment and support, and offer guidance on preventing future occurrences of vitamin A toxicity.
Tumor
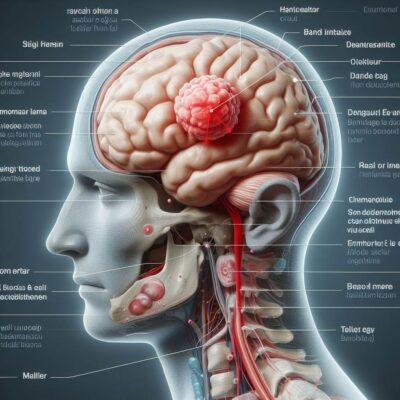
The term “tumor” often evokes fear and uncertainty, as it is commonly associated with cancer and serious medical conditions. However, tumors encompass a broader spectrum of growths, ranging from benign to malignant, and can occur in various tissues and organs throughout the body.
Understanding the nature of tumors, their potential causes, and the implications for health is essential for individuals seeking to navigate diagnosis, treatment, and overall well-being.
In this article, we’ll explore the topic of tumors, providing insights into their characteristics, types, and factors influencing their development. By shedding light on this complex subject, we aim to demystify tumors, empower individuals to advocate for their health, and foster greater awareness and understanding within the community.
Understanding Tumor:
1. Definition:
A tumor refers to an abnormal growth or mass of tissue that develops when cells multiply uncontrollably. Tumors can arise in any part of the body and may be benign (non-cancerous) or malignant (cancerous).
2. Types of Tumors:
Tumors are classified based on their characteristics and behavior. Benign tumors are typically localized, well-defined, and do not invade surrounding tissues or spread to other parts of the body. Malignant tumors, on the other hand, have the potential to invade nearby tissues and metastasize (spread) to distant organs, posing a greater risk to health.
3. Causes:
The causes of tumors vary depending on the type and location of the tumor. Some tumors may be genetic or hereditary, resulting from mutations in specific genes that regulate cell growth and division. Environmental factors such as exposure to carcinogens, radiation, or infectious agents may also contribute to tumor development.
4. Symptoms:
The symptoms of a tumor can vary widely depending on its size, location, and effects on surrounding tissues. Common symptoms may include pain, swelling, changes in bowel or bladder habits, unexplained weight loss, fatigue, and abnormal bleeding. However, some tumors may be asymptomatic and only detected through imaging studies or medical examinations.
5. Diagnosis:
Diagnosing a tumor typically involves a combination of medical history review, physical examination, imaging studies (such as X-rays, ultrasound, CT scans, or MRI), and laboratory tests (such as blood tests or biopsy) to evaluate the characteristics of the tumor and determine whether it is benign or malignant.
6. Treatment:
Treatment for tumors varies depending on factors such as the type, size, and location of the tumor, as well as the individual’s overall health and preferences. Options may include surgical removal of the tumor, radiation therapy, chemotherapy, immunotherapy, targeted therapy, or a combination of these approaches.
7. Prognosis:
The prognosis for individuals with tumors depends on factors such as the tumor’s type, stage, and response to treatment, as well as the individual’s overall health and other medical conditions. Benign tumors are generally associated with a good prognosis, while malignant tumors may have a more variable outcome depending on factors such as early detection and effective treatment.
8. Support and Resources:
Coping with a tumor diagnosis can be challenging, both emotionally and physically. It’s essential for individuals and their loved ones to seek support from healthcare professionals, support groups, and resources such as educational materials and counseling services to navigate the diagnosis, treatment, and recovery process.
How To Treat A Small Dent In Forehead After Hitting Head?

Accidents happen, and sometimes they result in unexpected bumps or bruises, including a small dent in the forehead after hitting the head. While this may cause concern, especially if it’s accompanied by other symptoms like headache or dizziness, there are steps you can take to address it effectively.
Knowing how to treat a small dent in the forehead after hitting the head can help alleviate discomfort and promote healing. In this article, we’ll explore practical tips and guidelines for treating a small dent in the forehead, whether it’s the result of a minor bump or a more significant head injury.
By understanding how to properly care for this type of injury, individuals can take proactive measures to ensure their well-being and minimize any potential complications.
Treat A Small Dent In Forehead:
1. Assess the Injury:
Before administering any treatment, it’s important to assess the severity of the injury. Determine if there are any accompanying symptoms such as headache, nausea, dizziness, or changes in consciousness, as these may indicate a more serious head injury requiring medical attention.
2. Apply Ice Packs:
If the injury is minor and there are no signs of a more serious head injury, applying an ice pack to the affected area can help reduce swelling and alleviate pain. Wrap the ice pack in a cloth or towel to protect the skin and apply it to the forehead for 15-20 minutes at a time, several times a day.
3. Use Pain Relievers:
Over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help manage any discomfort or headache associated with the injury. Follow the dosage instructions provided on the medication packaging and consult a healthcare provider if you have any concerns.
4. Monitor for Symptoms:
Keep a close eye on any symptoms that develop following the injury, especially if they worsen or persist over time. Symptoms such as persistent headache, vomiting, confusion, difficulty speaking or walking, or changes in vision may indicate a more serious head injury requiring medical evaluation.
5. Rest and Relaxation:
Encourage rest and relaxation to allow the body to recover from the injury. Avoid strenuous activities, sports, or heavy lifting that could exacerbate symptoms or delay healing. Get plenty of restorative sleep and prioritize self-care activities to support the body’s healing process.
6. Seek Medical Evaluation:
If the injury is more severe, if symptoms worsen or persist, or if there are concerns about a possible concussion or other head injury, seek prompt medical evaluation. A healthcare provider can assess the injury, perform necessary diagnostic tests, and recommend appropriate treatment based on the severity of the injury.
7. Follow Up:
After receiving medical evaluation and treatment, follow any recommendations provided by the healthcare provider for monitoring the injury and ensuring proper healing. Attend follow-up appointments as scheduled and communicate any changes in symptoms or concerns with the healthcare team.
8. Protective Measures:
Take precautions to prevent future head injuries, such as wearing protective headgear during sports or recreational activities, using seat belts and child safety seats in vehicles, and maintaining a safe environment free of hazards or obstacles that could cause falls or accidents.
Use A Cold Compress

When it comes to managing various injuries and ailments, sometimes the simplest solutions are the most effective. One such remedy that has stood the test of time is the use of a cold compress. Whether it’s a bump, bruise, or swelling, applying a cold compress can provide relief and promote healing.
Understanding the benefits and proper use of a cold compress can empower individuals to take proactive steps in managing minor injuries and discomfort. In this article, we’ll explore the use of a cold compress as a versatile and accessible treatment option.
From soothing headaches to reducing inflammation, a cold compress can be a valuable tool in your healthcare arsenal. Let’s delve into the benefits and best practices for using a cold compress to address a variety of common ailments and injuries.
Cold Compress:
1. Reduces Inflammation:
One of the primary benefits of using a cold compress is its ability to reduce inflammation. When applied to the affected area, the cold temperature causes blood vessels to constrict, which helps decrease swelling and inflammation.
2. Relieves Pain:
Cold therapy can also help alleviate pain associated with injuries, such as sprains, strains, or bruises. The numbing effect of the cold can temporarily dull pain receptors and provide relief from discomfort.
3. Soothes Headaches:
For individuals suffering from headaches or migraines, applying a cold compress to the forehead or temples can provide soothing relief. The cold temperature can help constrict blood vessels in the head, reducing blood flow and easing headache symptoms.
4. Promotes Healing:
By reducing inflammation and relieving pain, a cold compress can create an optimal environment for healing to occur. Whether it’s a minor injury or a post-surgical recovery, cold therapy can help expedite the healing process and improve outcomes.
5. Eases Muscle Soreness:
Athletes and fitness enthusiasts often use cold therapy to alleviate muscle soreness and speed up recovery after intense workouts. Applying a cold compress to sore muscles can help reduce inflammation and soothe discomfort, allowing for faster recovery and improved performance.
6. Alleviates Sunburn:
Sunburn can be painful and uncomfortable, but a cold compress can provide immediate relief. Applying a cold compress to sunburned skin can help cool the area, reduce inflammation, and alleviate pain and itching.
7. Reduces Puffiness:
Cold therapy can be beneficial for reducing puffiness and swelling around the eyes. Placing a cold compress over closed eyelids can help constrict blood vessels and reduce fluid retention, resulting in a refreshed and rejuvenated appearance.
8. Easy to Use:
One of the greatest advantages of a cold compress is its simplicity and convenience. Cold packs are readily available at pharmacies and can be easily stored in the freezer for quick access whenever needed. Alternatively, a makeshift cold compress can be created using ice cubes wrapped in a cloth or a bag of frozen vegetables.
Pain Relief Medication

Pain is a universal human experience, and finding relief from it is a common goal for many. Whether it’s a headache, muscle ache, or chronic condition, pain can significantly impact one’s quality of life. Pain relief medication, available in various forms and formulations, plays a crucial role in managing discomfort and restoring comfort and functionality.
From over-the-counter analgesics to prescription medications, the options for pain relief are vast and diverse. Understanding the different types of pain relief medication, their mechanisms of action, and when to use them can empower individuals to make informed choices about their pain management.
In this article, we’ll explore the world of pain relief medication, offering insights into its various forms, efficacy, and considerations for safe and effective use. Whether you’re dealing with acute pain or chronic discomfort, knowing your options for pain relief medication can make a significant difference in your overall well-being.
Medication:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
NSAIDs, such as ibuprofen (Advil, Motrin) and naproxen (Aleve), are commonly used to relieve pain and reduce inflammation. They work by inhibiting the production of prostaglandins, chemicals in the body that contribute to pain and inflammation.
2. Acetaminophen (Tylenol):
Acetaminophen is a pain reliever and fever reducer commonly used to alleviate mild to moderate pain. Unlike NSAIDs, acetaminophen does not have anti-inflammatory effects. It works by blocking pain signals in the brain and spinal cord.
3. Opioid Analgesics:
Opioids, such as oxycodone, hydrocodone, and morphine, are potent pain relievers used to manage moderate to severe pain. They work by binding to opioid receptors in the brain and spinal cord, blocking pain signals and producing feelings of euphoria and sedation.
4. Topical Pain Relievers:
Topical pain relievers, such as creams, gels, and patches, are applied directly to the skin over the painful area. They work by numbing the nerves in the skin and underlying tissues, providing localized pain relief.
5. Muscle Relaxants:
Muscle relaxants are medications used to alleviate muscle spasms and stiffness associated with conditions such as back pain and muscle injuries. They work by depressing the central nervous system and reducing muscle activity.
6. Antidepressants:
Certain antidepressant medications, such as tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs), are sometimes used to manage chronic pain conditions, such as neuropathic pain and fibromyalgia. They work by altering the levels of neurotransmitters in the brain involved in pain perception.
7. Anticonvulsants:
Anticonvulsant medications, such as gabapentin and pregabalin, are also used to treat certain types of chronic pain, including neuropathic pain and fibromyalgia. They work by stabilizing abnormal electrical activity in the brain and nerves associated with pain signaling.
8. Corticosteroids:
Corticosteroids, such as prednisone and dexamethasone, are powerful anti-inflammatory medications used to reduce inflammation and relieve pain associated with conditions such as arthritis, tendonitis, and inflammatory bowel disease.
Use Of Arnica Gel

Natural remedies have long been favored for their potential to provide relief from various ailments and discomforts. One such remedy that has gained popularity in recent years is arnica gel.
Derived from the Arnica montana plant, arnica gel is believed to possess anti-inflammatory and pain-relieving properties, making it a popular choice for alleviating muscle aches, bruises, and minor injuries. While scientific evidence supporting its effectiveness is limited, many individuals swear by arnica gel as a natural alternative to traditional pain relief medications.
Understanding the uses, benefits, and potential risks of arnica gel can help individuals make informed decisions about its incorporation into their healthcare routine. In this article, we’ll explore the use of arnica gel as a topical remedy, offering insights into its applications, efficacy, and considerations for safe and effective use.
Whether you’re seeking relief from sore muscles, bruises, or joint pain, arnica gel may offer a natural solution worth exploring.
Benefits Of Arnica Gel:
1. Relief from Muscle Aches:
Arnica gel is commonly used to alleviate muscle aches and soreness caused by strenuous exercise, overexertion, or injury. When applied topically to the affected area, arnica gel is believed to help reduce inflammation and promote relaxation of the muscles, leading to relief from discomfort.
2. Reduction of Bruising:
Arnica gel is often applied to bruises to help reduce swelling and discoloration. The anti-inflammatory properties of arnica may help speed up the healing process by increasing circulation to the affected area and facilitating the removal of pooled blood beneath the skin.
3. Management of Joint Pain:
Individuals experiencing joint pain, such as arthritis or minor joint injuries, may find relief from arnica gel. By applying the gel directly to the affected joints, individuals may experience temporary pain relief and improved mobility, although the extent of its efficacy varies among individuals.
4. Post-Surgical Recovery:
Arnica gel is sometimes used as part of the post-surgical recovery process to help manage pain, swelling, and bruising. Many individuals apply arnica gel to surgical incision sites to promote healing and minimize discomfort following procedures such as cosmetic surgery or dental extractions.
5. Sports Injuries:
Athletes and sports enthusiasts often use arnica gel to address minor injuries and muscle strains resulting from athletic activities. Applying arnica gel to injured muscles or joints may help reduce inflammation, alleviate pain, and support faster recovery, allowing individuals to return to their activities more quickly.
6. First Aid Treatment:
Arnica gel is a common addition to first aid kits for its potential to provide relief from minor injuries such as bumps, sprains, and strains. Its compact and portable nature makes it convenient for on-the-go use, whether at home, work, or during outdoor activities.
7. Considerations for Use:
While arnica gel is generally considered safe for topical use, it’s essential to follow the manufacturer’s instructions and guidelines for application. Avoid applying arnica gel to broken skin, mucous membranes, or near the eyes, as it may cause irritation or allergic reactions in some individuals.
8. Consultation with Healthcare Provider:
If you’re considering using arnica gel for a specific condition or injury, it’s advisable to consult with a healthcare provider, especially if you have underlying health conditions or are taking other medications. They can provide guidance on the appropriate use of arnica gel and offer recommendations tailored to your individual needs.
Gentle Massage

In the realm of self-care and wellness, few practices are as universally cherished as a gentle massage. Whether it’s a soothing touch from a loved one or a professional treatment at a spa, gentle massage offers a myriad of benefits for both the body and the mind.
From relieving muscle tension and promoting relaxation to improving circulation and reducing stress, the healing power of touch is undeniable. Incorporating gentle massage into your routine can be a simple yet effective way to nurture your physical and emotional well-being.
In this article, we’ll explore the practice of gentle massage, offering insights into its benefits, techniques, and considerations for incorporating it into your self-care regimen. Whether you’re seeking relief from muscle soreness, or tension headaches, or simply craving a moment of relaxation, gentle massage may hold the key to unlocking a world of comfort and rejuvenation.
Guide On Gentle Massage:
1. Relaxation:
One of the primary benefits of gentle massage is its ability to induce relaxation and reduce stress. The soothing touch of massage can help calm the nervous system, lower heart rate, and promote feelings of serenity and well-being.
2. Muscle Tension Relief:
Gentle massage can help alleviate muscle tension and stiffness, whether it’s caused by physical activity, poor posture, or stress. The rhythmic movements of massage help loosen tight muscles, improve flexibility, and restore range of motion.
3. Improved Circulation:
Massage stimulates blood flow to the muscles and tissues, promoting better circulation throughout the body. Improved circulation can enhance the delivery of oxygen and nutrients to cells, facilitate the removal of waste products, and promote overall health and vitality.
4. Pain Relief:
For individuals experiencing chronic pain conditions such as fibromyalgia, arthritis, or tension headaches, gentle massage can provide relief from discomfort. The release of endorphins during massage can help alleviate pain and promote feelings of comfort and well-being.
5. Stress Reduction:
Stress is a common culprit behind many health issues, including cardiovascular problems, digestive disorders, and weakened immune function. Gentle massage offers a natural and effective way to reduce stress levels, allowing the body and mind to relax and rejuvenate.
6. Improved Sleep Quality:
Many individuals find that gentle massage promotes better sleep quality and can help alleviate insomnia or sleep disturbances. The relaxation induced by massage can help calm the mind and body, making it easier to fall asleep and stay asleep throughout the night.
7. Emotional Healing:
Beyond its physical benefits, gentle massage can also have profound effects on emotional well-being. The nurturing touch of massage can promote feelings of comfort, security, and connection, fostering a sense of emotional balance and resilience.
8. Self-Care Practice:
Incorporating gentle massage into your self-care routine can be a powerful way to prioritize your health and well-being. Whether it’s a daily self-massage ritual or a weekly appointment with a massage therapist, taking time for gentle massage can provide a much-needed respite from the demands of daily life.
Hydration
Hydration is a cornerstone of good health, yet it’s a component of self-care that is often overlooked or underestimated. Our bodies are composed of approximately 60% water, and adequate hydration is essential for maintaining proper bodily functions, supporting metabolism, regulating body temperature, and promoting overall well-being.
However, many individuals fail to drink enough water throughout the day, leading to dehydration and its associated health consequences. Understanding the importance of hydration and adopting strategies to ensure adequate fluid intake is vital for optimizing health and vitality.
Hydration, delving into its benefits, signs of dehydration, and practical tips for staying properly hydrated. Whether you’re an athlete striving for peak performance, a busy professional juggling multiple responsibilities, or simply someone looking to enhance your health and well-being, prioritizing hydration is a fundamental step toward achieving your goals.
Guide On Hydration:
1. Optimal Physical Performance:
Proper hydration is crucial for maximizing physical performance and endurance. Dehydration can lead to decreased strength, endurance, and coordination, impairing athletic performance and increasing the risk of fatigue and injury.
2. Regulation of Body Temperature:
Water plays a vital role in regulating body temperature, particularly during exercise or exposure to hot and humid conditions. Adequate hydration helps the body sweat and dissipate heat, preventing overheating and heat-related illnesses such as heat exhaustion and heatstroke.
3. Supports Metabolism:
Hydration is essential for supporting metabolic processes within the body, including nutrient absorption, digestion, and waste elimination. Staying hydrated ensures optimal function of organs such as the kidneys, liver, and digestive system, promoting overall metabolic health.
4. Cognitive Function:
Dehydration can negatively impact cognitive function and mental performance, leading to symptoms such as impaired concentration, memory lapses, and mood changes. Maintaining proper hydration levels is essential for sustaining mental clarity, focus, and productivity.
5. Skin Health:
Adequate hydration is essential for maintaining healthy skin, as water helps hydrate skin cells, improve elasticity, and promote a youthful appearance. Dehydration can lead to dryness, flakiness, and premature aging of the skin, emphasizing the importance of staying hydrated for radiant and glowing skin.
6. Prevents Constipation:
Hydration plays a critical role in maintaining regular bowel movements and preventing constipation. Water helps soften stool, lubricate the digestive tract, and facilitate waste removal, promoting gastrointestinal health and preventing discomfort.
7. Supports Kidney Function:
Proper hydration is essential for supporting kidney function and preventing kidney stones and urinary tract infections. Adequate fluid intake helps flush out toxins and waste products from the body, reducing the risk of kidney-related issues and promoting urinary tract health.
8. Signs of Dehydration:
It’s important to recognize the signs of dehydration, which may include thirst, dry mouth, dark-colored urine, fatigue, dizziness, and headache. Severe dehydration can lead to symptoms such as rapid heartbeat, sunken eyes, confusion, and fainting, requiring immediate medical attention.
Give It Time For Small Dent In Forehead After Hitting Head
In today’s fast-paced world, patience can feel like a rare commodity. Whether it’s waiting for a career breakthrough, striving for personal growth, or seeking relief from a challenging situation, the instinct to rush and achieve immediate results is often strong.
However, there are moments in life when the most valuable action we can take is to simply give it time. Patience, perseverance, and trust in the process are essential virtues that allow us to navigate life’s uncertainties with grace and resilience.
Explore the concept of giving it time, examining its significance in various aspects of life, from personal development and relationships to career advancement and overcoming obstacles. By embracing the power of patience and allowing time to work its magic, we can cultivate a sense of peace, acceptance, and trust in the unfolding journey of life.
Give It Time Detail Guide:
1. Personal Growth:
Achieving personal growth and self-improvement often requires time and consistent effort. Whether it’s learning a new skill, breaking a habit, or healing from past traumas, giving yourself time to progress and evolve is essential for meaningful transformation.
2. Healing:
Emotional healing from loss, heartbreak, or trauma is a process that unfolds over time. While the pain may feel overwhelming in the moment, allowing yourself the space and patience to heal at your own pace is crucial for emotional well-being and resilience.
3. Relationships:
Building strong and meaningful relationships takes time and investment. Whether it’s forging new connections or repairing existing ones, giving relationships the time and attention they deserve fosters trust, understanding, and intimacy.
4. Career Advancement:
Advancing in your career and achieving professional goals often requires perseverance and patience. Success rarely happens overnight, and giving yourself time to learn, grow, and overcome challenges is essential for long-term success and fulfillment.
5. Overcoming Challenges:
When faced with obstacles or setbacks, it’s natural to feel frustrated or discouraged. However, giving yourself time to process your emotions, assess the situation, and develop a plan of action can help you overcome challenges with resilience and determination.
6. Creativity:
Creativity flourishes in an environment of patience and exploration. Whether it’s writing, painting, or pursuing other artistic endeavors, giving yourself the time and space to experiment, make mistakes, and refine your craft is essential for creative growth and expression.
7. Physical Health:
Achieving and maintaining physical health and fitness is a journey that unfolds over time. Consistent exercise, healthy eating habits, and self-care practices require patience and dedication, but the long-term benefits are well worth the investment.
8. Spiritual Growth:
Cultivating a deeper sense of spirituality and connection with the universe is a lifelong journey that unfolds gradually. Giving yourself the time and space for introspection, meditation, and self-discovery can lead to profound insights and personal transformation.
Diagnosis And When To See A Doctor Regarding (Small Dent In Forehead After Hitting Head)
Navigating health concerns can be a daunting experience, especially when symptoms arise that cause uncertainty or distress. In such instances, understanding when to seek medical attention and obtain a diagnosis is crucial for timely intervention and appropriate treatment.
While some symptoms may be minor and resolve on their own, others may indicate underlying health issues that require professional evaluation. Knowing when to see a doctor can help individuals address health concerns proactively, leading to better outcomes and improved well-being.
Let’s understand the importance of diagnosis and when to seek medical attention for symptoms or health issues. By recognizing the signs that warrant medical evaluation and understanding the diagnostic process, individuals can take proactive steps to prioritize their health and receive the care they need promptly.
To See A Doctor:
1. Persistent Symptoms:
If you experience persistent symptoms that don’t improve or worsen over time, it’s important to seek medical attention. Examples include chronic pain, persistent cough, unexplained weight loss, or changes in bowel habits.
2. Severe Symptoms:
Severe symptoms such as sudden chest pain, difficulty breathing, severe headache, or loss of consciousness require immediate medical attention and evaluation.
3. New or Unusual Symptoms:
Any new or unusual symptoms that arise without explanation should be evaluated by a healthcare professional. This includes symptoms such as lumps or masses, changes in vision or hearing, or unexplained fatigue.
4. Changes in Functionality:
If you experience changes in your ability to perform daily activities or tasks, such as difficulty walking, speaking, or swallowing, it’s important to consult with a doctor to determine the underlying cause.
5. Family History:
Individuals with a family history of certain medical conditions or diseases may be at higher risk and should be vigilant about seeking medical evaluation for symptoms or changes in health status.
6. Routine Screenings:
Regular health screenings and check-ups are essential for early detection of potential health issues. Even in the absence of symptoms, it’s important to follow recommended screening guidelines for conditions such as cancer, heart disease, diabetes, and hypertension.
7. Diagnostic Tests:
If your doctor suspects an underlying health issue based on your symptoms and medical history, they may order diagnostic tests such as blood tests, imaging studies, or biopsies to confirm a diagnosis and develop an appropriate treatment plan.
8. Trust Your Instincts:
Ultimately, if you’re concerned about your health or have a gut feeling that something isn’t right, don’t hesitate to seek medical attention. Trusting your instincts and advocating for your health is essential for obtaining timely diagnosis and treatment.
Dent In Skull After Hitting Head For Child?
As parents, ensuring the safety and well-being of our children is a top priority. However, accidents and injuries can occur, often leaving us feeling anxious and unsure about the best course of action. One such concern that may arise is the presence of a dent in the skull after a child has experienced a head injury.
While it’s natural to feel concerned, it’s essential to approach the situation with clarity and understanding. In this article, we’ll explore the potential causes of a dent in the skull after a child has hit their head, as well as when it’s advisable to seek medical attention.
By understanding the factors at play and knowing when to take action, parents can ensure the health and safety of their children in the event of a head injury.
What To Do When Dent in Skull After Hitting Head for Child:
1. Bone Structure:
In some cases, the presence of a dent in the skull may be due to the natural variation in bone structure. Just as adults may have irregularities in the shape of their skull, children may also exhibit variations that are not necessarily indicative of an injury or underlying health issue.
2. Soft Spot Closure:
Infants have soft spots on their skulls called fontanelles, which allow for flexibility during childbirth and early brain development. As these fontanelles close over time, they may leave behind slight depressions or dents in the skull, which are typically harmless.
3. Cephalohematoma:
A cephalohematoma is a collection of blood beneath the skull’s periosteum, often resulting from trauma during childbirth. While a cephalohematoma may cause a noticeable lump or swelling on the baby’s head, it usually resolves on its own over several weeks to months and does not require treatment.
4. Skull Fracture:
In more severe cases, a dent in the skull may indicate a skull fracture resulting from a significant impact or trauma to the head. Symptoms of a skull fracture may include swelling, bruising, tenderness, and changes in consciousness. If you suspect a skull fracture or if your child exhibits any concerning symptoms after a head injury, seek medical attention immediately.
5. Concussion:
A concussion is a mild traumatic brain injury that occurs when the brain is jolted or shaken inside the skull. While concussions do not typically cause visible dents or deformities in the skull, they can result in symptoms such as headache, dizziness, nausea, and confusion. If your child experiences a head injury and exhibits symptoms of a concussion, it’s important to seek medical evaluation.
6. Observation:
In many cases, a minor bump or bruise to the head may not cause any serious injury and can be managed with observation at home. However, if you notice any concerning symptoms such as persistent vomiting, changes in behavior, difficulty walking, or loss of consciousness, seek medical attention immediately.
7. Medical Evaluation:
If you’re uncertain about the severity of your child’s head injury or if they exhibit any concerning symptoms, it’s always best to err on the side of caution and seek medical evaluation. A healthcare provider can assess the extent of the injury, perform any necessary diagnostic tests, and provide appropriate treatment or recommendations for further care.
8. Prevention:
While accidents are sometimes unavoidable, taking steps to prevent head injuries can help protect your child’s safety. Ensure that your home is childproofed to minimize the risk of falls, use appropriate safety gear during recreational activities, and supervise young children closely to prevent accidents.
Conclusion:
Experiencing a small dent in the forehead after hitting the head can be a cause for concern, but it’s important to approach the situation calmly and rationally. While it may be unsettling to notice a physical change in the skull, such as a dent, it’s essential to assess the severity of the injury and seek appropriate medical attention if needed.
In many cases, a minor bump or bruise to the head may not cause any serious harm and can be managed with observation at home. However, if there are any concerning symptoms or if the dent is accompanied by other signs of a head injury, such as persistent pain, swelling, or changes in consciousness, it’s crucial to seek medical evaluation promptly.
By prioritizing safety and seeking medical advice when necessary, individuals can ensure the health and well-being of themselves or their loved ones in the event of a head injury. I hope now you have “Small Dent In Forehead After Hitting Head”.
FAQs:
Q1: What should I do if my child develops a small dent in their forehead after hitting their head?
A: If your child experiences a head injury and develops a small dent in their forehead, it’s essential to assess the severity of the injury and monitor for any concerning symptoms. If there are any signs of a concussion or other head injury, such as persistent pain, swelling, or changes in consciousness, seek medical attention promptly.
Q2: Can a small dent in the forehead heal on its own?
A: In some cases, a small dent in the forehead may heal on its own over time, especially if it’s the result of a minor bump or bruise to the head. However, if there are any signs of a more serious head injury or if the dent is accompanied by other concerning symptoms, it’s important to seek medical evaluation. “Small Dent In Forehead After Hitting Head”
Q3: What are the potential causes of a small dent in the forehead after hitting the head?
A: A small dent in the forehead after hitting the head may be caused by various factors, including natural variations in bone structure, trauma to the skull, or underlying medical conditions. In some cases, it may be a harmless cosmetic issue, while in others, it may require medical evaluation and treatment. “Small Dent In Forehead After Hitting Head”
Q4: How can I tell if a small dent in the forehead is a sign of a more serious head injury?
A: Signs that a small dent in the forehead may be indicative of a more serious head injury include persistent pain, swelling, bruising, changes in consciousness, vomiting, or difficulty walking. If any of these symptoms are present, seek medical attention promptly. “Small Dent In Forehead After Hitting Head”
Q5: What can I do to prevent head injuries in the future?
A: To reduce the risk of head injuries, especially in children, take precautions such as childproofing the home to minimize the risk of falls, using appropriate safety gear during recreational activities, and supervising young children closely to prevent accidents. Additionally, encourage safe behavior and educate children about the importance of wearing helmets and avoiding risky activities. “Small Dent In Forehead After Hitting Head”
