
Gingivitis, a common yet often overlooked oral health issue, is an early stage of gum disease characterized by inflammation of the gums. Despite its prevalence, many individuals remain unaware of its initial signs and potential severity if left untreated.
Gingivitis is typically caused by the accumulation of plaque—a sticky film of bacteria—on the teeth. Poor oral hygiene practices can exacerbate this condition, leading to swollen, red, and bleeding gums. However, the good news is that gingivitis is both preventable and reversible with proper care. Early detection and consistent oral hygiene routines are crucial in managing and eliminating this ailment.
Understanding the nuances of gingivitis is essential for maintaining overall dental health and preventing more serious complications, such as periodontitis.
What Is Gingivitis

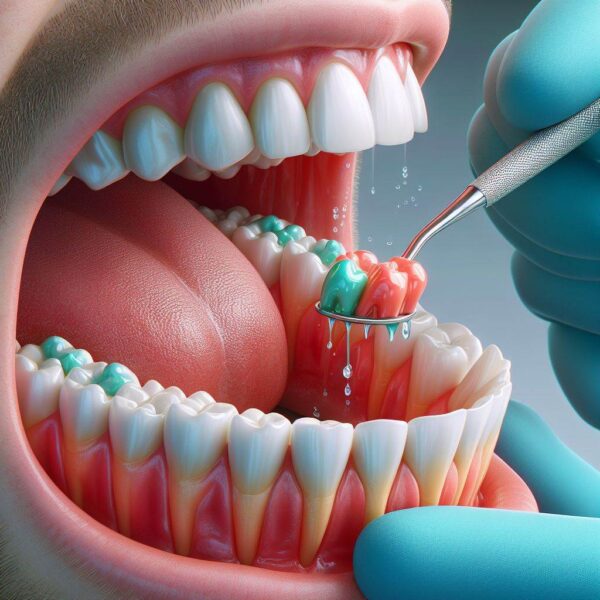
Gingivitis is primarily instigated by the accumulation of plaque on the teeth and gum line. Plaque forms when food particles and bacteria mix, creating a sticky substance that adheres to the teeth. If not removed through regular brushing and flossing, plaque can harden into tartar, which can only be removed by a dental professional.
The presence of tartar irritates the gums, leading to inflammation and the early stages of gum disease. Common symptoms of gingivitis include red, swollen gums, bleeding during brushing or flossing, and persistent bad breath.
In some cases, the gums may recede, making the teeth appear longer than usual. Recognizing these signs early and seeking appropriate dental care can prevent the progression to more severe forms of gum disease. I hope now you are aware of what is gingivitis.
What Causes Gingivitis?
Gingivitis, a prevalent yet often unnoticed dental condition, signifies the early stage of gum disease characterized by inflammation and irritation of the gums. Many people experience gingivitis without realizing its root causes, leading to more severe dental problems if left unaddressed.
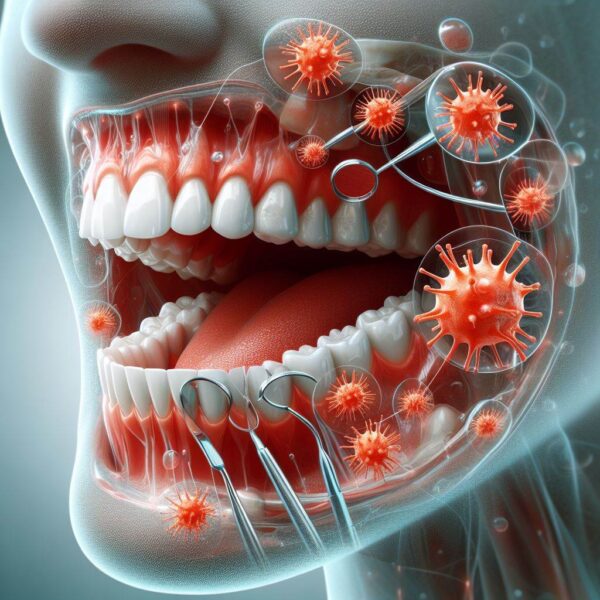
Understanding what triggers gingivitis is crucial for effective prevention and treatment. Typically, this condition arises from the accumulation of plaque—a sticky film of bacteria on the teeth and gums.
However, several other factors can contribute to the development of gingivitis, including poor oral hygiene, certain lifestyle habits, and underlying health conditions. By recognizing and addressing these causes, individuals can take proactive steps to maintain optimal oral health and prevent the progression of gum disease.
Key Factors Leading to Gingivitis
Poor Oral Hygiene Practices:
Inadequate brushing and flossing allow plaque to accumulate on the teeth and gum line. Over time, this buildup irritates the gums, leading to inflammation and bleeding.
Plaque and Tartar Buildup:
Plaque forms when bacteria in the mouth mix with food particles. If not removed, it hardens into tartar, which can only be eliminated by a dental professional. Tartar irritates the gums, causing gingivitis.
Tobacco Use:
Smoking or chewing tobacco can significantly increase the risk of developing gingivitis. Tobacco products hinder the healing process of gum tissue and contribute to the accumulation of plaque.
Hormonal Changes:
Hormonal fluctuations during pregnancy, menstruation, or menopause can make gums more sensitive and prone to inflammation, increasing the likelihood of gingivitis.
Certain Medications:
Some medications reduce saliva flow, leading to dry mouth. Saliva helps protect the gums and teeth from bacteria, and its reduction can create an environment conducive to gingivitis.
Health Conditions:
Diseases such as diabetes, cancer, and HIV/AIDS can compromise the immune system, making it harder for the body to fight off infections, including those that cause gum disease.
Nutritional Deficiencies:
A diet lacking in essential nutrients, particularly vitamin C, can weaken the gums and make them more susceptible to infection and inflammation.
Gingivitis Treatment

Gingivitis, the initial stage of gum disease, often goes unnoticed until symptoms like red, swollen, and bleeding gums appear. This condition arises due to the accumulation of plaque, a sticky film of bacteria, on the teeth and gum line.
If left untreated, gingivitis can progress to more severe forms of periodontal disease, leading to tooth loss and other health issues.
The good news is that gingivitis is both preventable and treatable with proper care. Understanding the various treatment options available can help in reversing this condition and maintaining optimal oral health.
This article explores effective treatments for gingivitis, providing valuable insights to keep your gums healthy.
Primary Treatments for Gingivitis
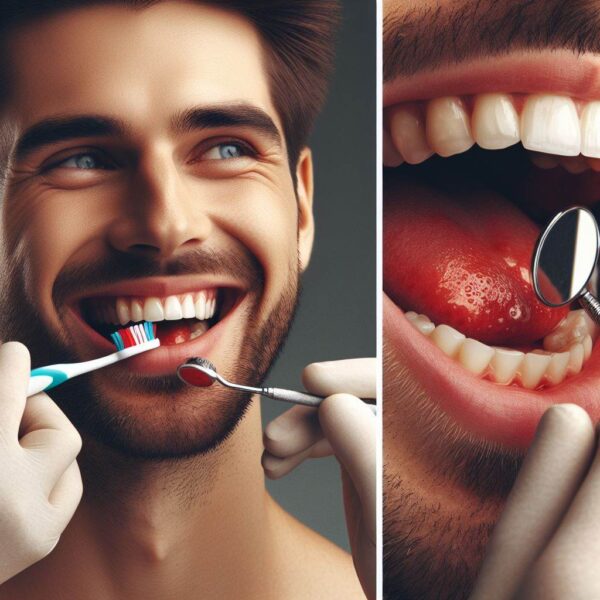
Enhanced Oral Hygiene:
Brush your teeth at least twice a day with fluoride toothpaste. Use a soft-bristled toothbrush to avoid irritating your gums.
Floss daily to remove plaque and food particles from between your teeth and along the gum line where a toothbrush cannot reach.
Professional Dental Cleaning:
Regular dental check-ups and cleanings are crucial. Dentists can remove tartar (hardened plaque) that brushing and flossing alone cannot eliminate.
Professional cleanings help to prevent the progression of gingivitis and maintain gum health.
Antiseptic Mouthwash:
Using an antiseptic mouthwash can help reduce the bacterial load in your mouth, thus controlling plaque and reducing gum inflammation.
Over-the-counter and prescription options are available based on the severity of the condition.
Scaling and Root Planing:
For more advanced cases, a deep cleaning procedure called scaling and root planing might be necessary. This involves removing plaque and tartar from below the gum line and smoothing the root surfaces to promote healing.
Antibiotic Therapy:
In cases where bacterial infection is significant, dentists may prescribe antibiotics. These can be in the form of mouth rinses, gels applied to the gum pockets, or oral tablets.
Lifestyle Changes:
Quitting smoking and avoiding tobacco products can significantly improve gum health.
Adopting a balanced diet rich in vitamins and minerals, particularly vitamin C and calcium, supports gum health and aids in recovery from gingivitis.
Long-term Maintenance and Prevention:
Maintaining healthy gums requires ongoing care even after treating gingivitis. Regular dental visits, at least twice a year, are essential to monitor oral health and prevent recurrence.
Consistently practicing good oral hygiene and addressing any underlying health conditions can help sustain gum health. Additionally,
being attentive to changes in your gums and seeking prompt dental advice if symptoms reappear can prevent the condition from progressing.
Gingivitis Side Effect

Gingivitis, the early stage of gum disease, is commonly characterized by symptoms such as swollen, red, and bleeding gums. While it might seem like a minor issue, gingivitis can lead to several adverse effects if not addressed promptly.
These side effects extend beyond oral health, potentially impacting overall well-being. As plaque accumulates on the teeth and gums, it triggers an inflammatory response, which can have various repercussions.
Recognizing and understanding the side effects of gingivitis is crucial for effective management and prevention. This article delves into the potential side effects of gingivitis, highlighting the importance of early intervention and consistent oral care.
Key Side Effects of Gingivitis
Periodontitis Development:
If gingivitis is left untreated, it can progress to periodontitis, a more severe form of gum disease. Periodontitis involves deeper infection and damage to the supporting structures of the teeth, leading to tooth loss.
Gum Recession:
Gingivitis can cause the gums to recede, exposing the roots of the teeth. This not only increases sensitivity to hot and cold but also creates pockets where bacteria can accumulate, exacerbating the problem.
Bad Breath (Halitosis):
Chronic bad breath is a common side effect of gingivitis. The buildup of plaque and bacteria in the mouth produces foul-smelling compounds, leading to persistent bad breath.
Tooth Sensitivity:
As the gums become inflamed and recede, the exposed tooth roots can lead to increased sensitivity. This can make eating and drinking hot, cold, or sweet foods uncomfortable.
Bleeding Gums:
One of the earliest signs of gingivitis is bleeding gums, especially during brushing or flossing. Persistent bleeding indicates ongoing inflammation and damage to the gum tissues.
Increased Risk of Systemic Health Issues:
Emerging research suggests a link between gum disease and systemic health problems, including heart disease, diabetes, and respiratory issues. The inflammation associated with gingivitis can contribute to the overall inflammatory burden on the body.
Loose Teeth:
As gingivitis progresses to periodontitis, the supporting structures of the teeth, including the bone, can deteriorate. This can result in loose teeth and eventually tooth loss if not treated.
What Is The Main Cause Of Gingivitis?
Gingivitis, the earliest stage of gum disease, often presents with symptoms like red, swollen, and bleeding gums. It’s a widespread condition that can lead to more severe dental issues if not treated promptly.
The primary cause of gingivitis is the buildup of plaque—a sticky film of bacteria—on the teeth and gums. While poor oral hygiene is the main culprit, other factors can also contribute to the development of gingivitis.
By understanding what triggers this condition, individuals can take preventive measures to maintain their oral health and avoid the progression of gum disease. This article explores the primary cause of gingivitis and highlights the steps needed to prevent it.
Primary Cause of Gingivitis: Plaque Buildup
Poor Oral Hygiene:
Inadequate brushing and flossing habits allow plaque to accumulate on the teeth and along the gum line. This buildup irritates the gums, leading to inflammation and the initial stages of gingivitis.
Plaque Formation:
Plaque is a colorless, sticky film that forms on teeth when bacteria in the mouth mix with food particles. If not removed regularly through brushing and flossing, plaque hardens into tartar, which further irritates the gums.
Diet and Nutrition:
Diets high in sugar and carbohydrates contribute to plaque formation. Bacteria feed on these sugars, producing acids that irritate the gums and enamel.
Smoking and Tobacco Use:
Tobacco products contribute to the buildup of plaque and tartar on teeth, and they also impair the immune system, making it harder for the body to fight off a gum infection.
Hormonal Changes:
Hormonal fluctuations during pregnancy, puberty, menstruation, and menopause can make gums more sensitive and susceptible to gingivitis.
Medical Conditions:
Diseases such as diabetes and conditions that weaken the immune system can increase the risk of developing gingivitis. These conditions can reduce the body’s ability to fight off infections, including gum infections.
Medications:
Certain medications that reduce saliva flow can lead to dry mouth, which creates an environment where plaque is more likely to form. Saliva is essential in washing away food particles and neutralizing acids produced by bacteria.
What 3 Symptoms Are Present With Gingivitis?
Gingivitis, the early stage of gum disease, often manifests with several noticeable symptoms that indicate an underlying oral health issue. Identifying these symptoms early is crucial for prompt intervention and preventing the progression of gum disease to more severe stages.
While gingivitis can present with various signs, there are three key symptoms that commonly accompany this condition. Understanding and recognizing these symptoms can empower individuals to take proactive steps in addressing gingivitis and maintaining optimal oral health.
This article explores the three primary symptoms associated with gingivitis, providing valuable insights to help you identify and address this common dental concern.
Common Symptoms of Gingivitis
Swollen Gums
One of the hallmark symptoms of gingivitis is gum inflammation, resulting in swelling and puffiness. Healthy gums are firm and pink, but when affected by gingivitis, they may appear red, tender, and swollen.
Bleeding Gums
Another telltale sign of gingivitis is bleeding gums, particularly during brushing or flossing. Healthy gums typically do not bleed during routine oral care practices. If you notice blood when brushing or flossing, it could indicate gingivitis or another underlying issue.
Gum Sensitivity
Individuals with gingivitis may experience increased sensitivity or discomfort in their gums, especially when pressure is applied, such as while chewing or brushing. The gums may feel tender or sore to the touch, indicating inflammation and irritation.
Is Gingivitis Very Bad?
Gingivitis, although common, is often underestimated in terms of its potential impact on oral health. Many individuals may wonder about the severity of gingivitis and whether it poses a significant risk.
While gingivitis itself is considered a mild form of gum disease, it can lead to more serious complications if left untreated. Understanding the implications of gingivitis is essential for maintaining optimal oral health and preventing further issues down the line.
In this article, we’ll delve into the question of whether gingivitis is truly “very bad” and shed light on why early intervention and proper management are crucial in addressing this dental concern.
Is Gingivitis Very Bad?
Gingivitis, in its early stages, may not seem very severe compared to other health conditions. However, dismissing gingivitis as a minor issue can be misleading. While it may not cause immediate pain or discomfort, untreated gingivitis can progress to more advanced forms of gum disease, such as periodontitis.
This can lead to irreversible damage to the gums, bone loss, and even tooth loss over time. Additionally, research suggests a potential link between gum disease and systemic health issues, including heart disease, diabetes, and respiratory problems.
Therefore, while gingivitis itself may not be considered “very bad” in the traditional sense, its implications for overall health should not be underestimated.
Taking proactive steps to address gingivitis, such as maintaining good oral hygiene, seeking regular dental care, and addressing risk factors like smoking or certain medical conditions, is essential in preventing further complications and preserving oral and systemic health.
How Is Gingivitis Diagnosed?

Gingivitis, an early stage of gum disease, often lurks beneath the surface, making its diagnosis a critical aspect of dental care. While it may not always present with obvious symptoms, timely detection is key to preventing its progression into more severe conditions.
Dentists employ a variety of methods to diagnose gingivitis accurately, ensuring prompt intervention and treatment. Understanding how gingivitis is diagnosed empowers individuals to prioritize their oral health and seek timely dental care.
In this article, we’ll explore the diagnostic journey for gingivitis, shedding light on the techniques and approaches utilized by dental professionals to identify this common oral ailment.
The Diagnostic Process Unveiled
Visual Examination:
Dentists conduct a thorough visual inspection of the gums, looking for signs of inflammation, swelling, and discoloration. They also assess the overall condition of the gum tissue.
Probing of the Gums:
Using a periodontal probe, dentists measure the depth of the gum pockets around each tooth. Increased pocket depth may indicate gum disease, including gingivitis.
Evaluation of Symptoms:
Dentists inquire about any symptoms the individual may be experiencing, such as bleeding gums, bad breath, or gum sensitivity. These symptoms can provide valuable clues to the presence of gingivitis.
Review of Medical History:
Dentists review the individual’s medical history to identify any underlying health conditions or risk factors that may contribute to gum disease. Certain systemic conditions, medications, and lifestyle factors can impact oral health.
Additional Diagnostic Tests:
In some cases, dentists may recommend additional diagnostic tests, such as dental X-rays, to assess the extent of gum and bone damage. X-rays can reveal hidden signs of gum disease that may not be apparent during a visual examination.
Can Gingivitis Be Prevented?

Gingivitis, the initial stage of gum disease, may seem like a minor concern, but its potential impact on oral health should not be underestimated. Fortunately, proactive measures can significantly reduce the risk of developing gingivitis and help maintain healthy gums.
By adopting proper oral hygiene practices and making lifestyle adjustments, individuals can take charge of their oral health and prevent the onset of gingivitis. Understanding the strategies for preventing gingivitis empowers individuals to prioritize their oral care and avoid the complications associated with gum disease.
In this article, we’ll delve into the various preventive measures that can help keep gingivitis at bay, ensuring a healthier smile and overall well-being.
Preventing Gingivitis: A Comprehensive Approach
Maintain Excellent Oral Hygiene: Brushing your teeth at least twice a day with fluoride toothpaste and flossing daily are essential for removing plaque and preventing its buildup along the gumline.
Regular Dental Check-ups:
Schedule routine dental visits every six months for professional cleanings and check-ups. Dentists can detect early signs of gingivitis and provide personalized recommendations for oral care.
Healthy Lifestyle Choices:
Avoid tobacco products, which can increase the risk of gum disease. Adopt a balanced diet rich in fruits, vegetables, and lean proteins to support gum health.
Manage Underlying Health Conditions:
Certain systemic conditions, such as diabetes, can increase the risk of gum disease. Proper management of these conditions, along with regular dental care, can help prevent gingivitis.
Stay Hydrated:
Drink plenty of water throughout the day to maintain saliva production, which helps wash away food particles and bacteria that can contribute to gum disease.
Is Gingivitis Contagious?

Gingivitis, an inflammation of the gums often associated with poor oral hygiene, prompts questions about its contagious nature. Many wonder if this common dental condition can spread from person to person, especially in close social settings.
Understanding the contagiousness of gingivitis is essential for dispelling myths and ensuring accurate information regarding oral health. By exploring this topic, individuals can take proactive steps to protect themselves and their loved ones from the potential risks associated with gum disease transmission.
In this article, we’ll delve into the question of whether gingivitis is contagious, providing clarity on this often misunderstood aspect of dental health.
Debunking the Myth: Is Gingivitis Contagious?
Contrary to common misconceptions, gingivitis itself is not directly contagious in the traditional sense. Unlike infectious diseases like the flu or cold, gingivitis does not spread through casual contact or airborne particles.
However, the bacteria that contribute to gum disease can be transmitted between individuals through activities such as sharing utensils, intimate contact, or even kissing.
While the transmission of gingivitis is not as straightforward as that of a viral infection, close contact with someone who has untreated gum disease can increase the risk of bacterial transfer.
Therefore, while gingivitis is not inherently contagious, preventive measures such as maintaining good oral hygiene and avoiding behaviors that can facilitate bacterial spread are essential for preventing its transmission.
Increasing public awareness about the factors contributing to gum disease and promoting education about oral hygiene can help dispel misconceptions and ensure accurate information regarding gingivitis transmission.
By taking proactive steps to maintain oral health and seeking timely treatment for gum disease, individuals can protect themselves and others from the potential risks associated with bacterial transmission within their communities.
Gingivitis During Pregnancy

Pregnancy is a time of joy and anticipation, but it also brings about changes in the body, including potential impacts on oral health. Gingivitis, a common gum disease characterized by inflammation, can become more prevalent during pregnancy due to hormonal fluctuations and other factors.
Addressing gingivitis during pregnancy is crucial not only for the mother’s oral health but also for the well-being of the baby.
This comprehensive guide explores the relationship between pregnancy and gingivitis, providing valuable insights and practical tips for expectant mothers to maintain optimal oral health throughout their pregnancy journey.
The Connection Between Pregnancy and Gingivitis
Hormonal Changes:
Increased levels of progesterone during pregnancy can make gums more sensitive to plaque, leading to inflammation and gingivitis.
Increased Risk Factors:
Morning sickness, hormonal changes, and cravings for sugary foods can contribute to an increased risk of gum disease during pregnancy.
Potential Complications:
Gingivitis during pregnancy has been linked to adverse pregnancy outcomes such as preterm birth and low birth weight, highlighting the importance of addressing gum disease during this time.
Managing Gingivitis During Pregnancy: Practical Tips
Maintain Good Oral Hygiene:
Brush teeth at least twice a day with fluoride toothpaste and floss daily to remove plaque and bacteria.
Regular Dental Check-ups:
Schedule dental visits for professional cleanings and check-ups, informing your dentist of your pregnancy.
Address Changes in Oral Health:
Report any changes in oral health, such as bleeding gums or increased sensitivity, to your dentist promptly.
Balanced Diet:
Adopt a balanced diet rich in fruits, vegetables, and calcium to support gum health and overall well-being.
Stay Hydrated:
Drink plenty of water to maintain saliva production, which helps wash away food particles and bacteria.
Avoid Tobacco Products:
Refrain from using tobacco products, as they can exacerbate gum inflammation and increase the risk of gum disease.
Manage Stress:
Practice stress-reducing techniques such as meditation or gentle exercise to help maintain overall health and well-being during pregnancy.
Conclusion
Gingivitis is a preventable and treatable condition that underscores the importance of maintaining good oral hygiene practices. By understanding the symptoms, causes, and treatments associated with gingivitis, individuals can take proactive measures to protect their gum health.
Early detection and consistent care are vital to reversing gingivitis and preventing it from developing into more severe periodontal diseases. Regular dental visits and proper daily oral care routines are essential in ensuring healthy gums and overall oral well-being. I hoe now your are fully aware of everything about the topic what is gingivitis.
FAQs:
Q1. How does gingivitis differ from periodontitis?
A1. Gingivitis is the inflammation of the gums without affecting the bone, whereas periodontitis is a more severe gum disease that involves inflammation and infection that damages the bone and tissues supporting the teeth. Gingivitis can be reversed with proper care, but untreated gingivitis can progress to periodontitis, leading to tooth loss and more serious health issues.
Q2. What are the early signs of gingivitis?
A2. The early signs of gingivitis include redness and swelling of the gums, bleeding during brushing or flossing, and persistent bad breath. These symptoms may be mild and easily overlooked, so regular dental check-ups are important for early detection and treatment.
Q3. Can gingivitis affect overall health?
A3. Yes, gingivitis can affect overall health. Studies have shown links between gum disease and systemic conditions such as heart disease, diabetes, and respiratory issues. Maintaining good oral health is not only vital for preventing gum disease but also for protecting overall health.
Q4. What lifestyle changes can help prevent gingivitis?
A4. Several lifestyle changes can help prevent gingivitis, including quitting smoking, maintaining a balanced diet rich in vitamins and minerals, managing stress, and ensuring adequate hydration. These changes support overall health and reduce the risk of gum disease.
Q5. Are there any specific foods that can help combat gingivitis?
A5. Yes, certain foods can help combat gingivitis. Foods rich in vitamin C, such as citrus fruits, strawberries, and leafy greens, can strengthen gums and prevent inflammation. Crunchy vegetables like carrots and celery can help clean teeth and stimulate gums. Incorporating these foods into your diet can aid in maintaining healthy gums and preventing gingivitis.
