Embarking on the journey of oral health, one inevitably encounters the intricate stages of periodontal disease, a common yet often underestimated dental condition affecting countless individuals worldwide.
Recognizing and understanding the distinct stages of this ailment is paramount for maintaining optimal oral hygiene and preventing serious complications.
In this comprehensive guide, we delve into the diverse phases of periodontal disease, shedding light on their characteristics and implications, to equip readers with the knowledge needed to safeguard their dental well-being effectively.
What Are The Stages Of Periodontal Disease

Periodontal disease, a common yet often underestimated oral health concern, affects millions worldwide. Its progression unfolds in stages, each presenting unique challenges and implications for dental health.
Understanding these stages is crucial for effective prevention and treatment. In this article, we delve into the intricate journey of periodontal disease, shedding light on its various stages and their impact on oral well-being.
Exploring The Stages:
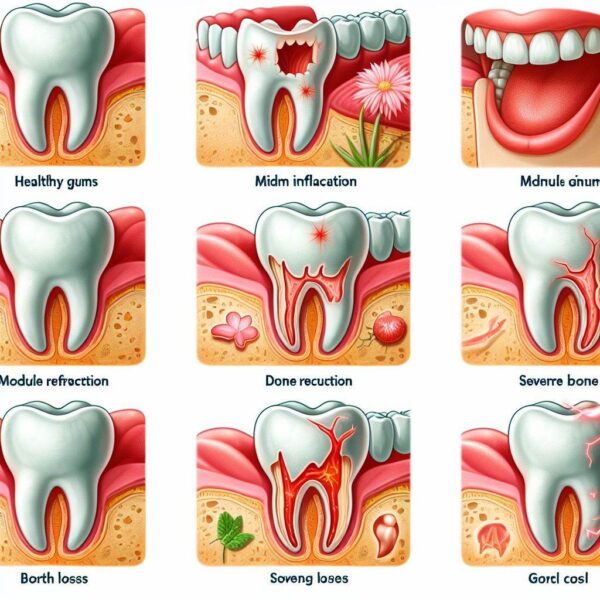
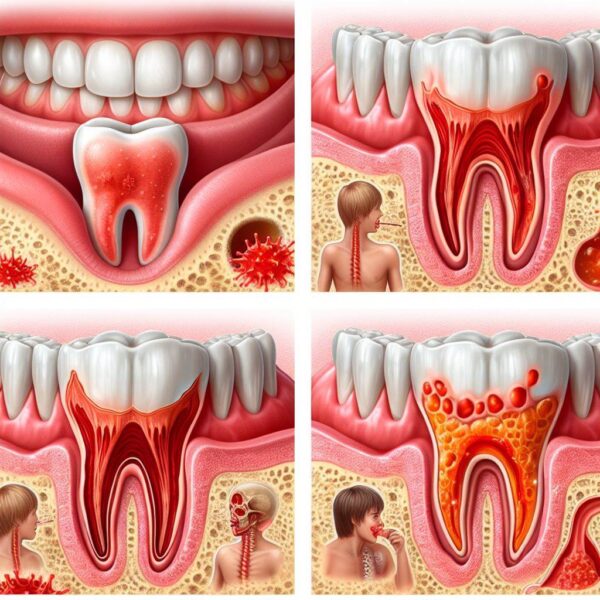
Stage 1: Gingivitis
Characterized by inflammation of the gums.
Symptoms include redness, swelling, and bleeding during brushing or flossing.
Gingivitis is reversible with proper oral hygiene and professional treatment.
Stage 2: Early Periodontitis
Progression of gingivitis into early periodontitis involves the formation of pockets between the gums and teeth.
Gums may recede, and bone loss can begin.
Halitosis (bad breath) and tooth sensitivity may develop.
Stage 3: Moderate Periodontitis
Increased pocket depth, leading to further bone and tissue loss.
Teeth may become loose, affecting bite and chewing ability.
Visible changes in tooth positioning and appearance may occur.
Stage 4: Advanced Periodontitis
Severe damage to the bone and supporting tissues.
Tooth mobility is significant, and tooth loss becomes likely.
Advanced periodontitis can impact overall health, contributing to systemic conditions like cardiovascular disease. I hope you understand about What Are The Stages Of Periodontal Disease.
What Is Stage 4 Periodontal Disease?
Stage IV periodontal disease, also known as advanced periodontitis, represents the most severe form of gum disease and poses significant risks to oral health and overall well-being.
Characterized by extensive damage to the supporting structures of the teeth, stage IV periodontal disease demands immediate attention and comprehensive treatment.
In this article, we delve into the intricacies of stage IV periodontal disease, exploring its causes, symptoms, and available treatment options to provide readers with valuable insights into this critical dental condition.
Exploring Stage IV Periodontal Disease:
Stage IV periodontal disease is the most advanced stage of gum disease, marked by profound destruction of the bone and soft tissues that support the teeth.
At this stage, the gums may recede significantly, exposing the roots of the teeth and leading to increased tooth mobility. Deep pockets form between the teeth and gums, harboring harmful bacteria that further exacerbate the condition.
Causes of Stage IV Periodontal Disease:
Several factors contribute to the development and progression of stage IV periodontal disease. Poor oral hygiene habits, including inadequate brushing and flossing, allow plaque and tartar to accumulate along the gumline, leading to inflammation and infection.
Smoking and tobacco use are significant risk factors for periodontal disease, as they impair blood flow to the gums and weaken the immune system’s ability to fight off infections.
Additionally, genetic predisposition, hormonal changes, and certain medical conditions, such as diabetes, can increase the likelihood of developing advanced gum disease.
What Is Stage 5 Periodontitis?
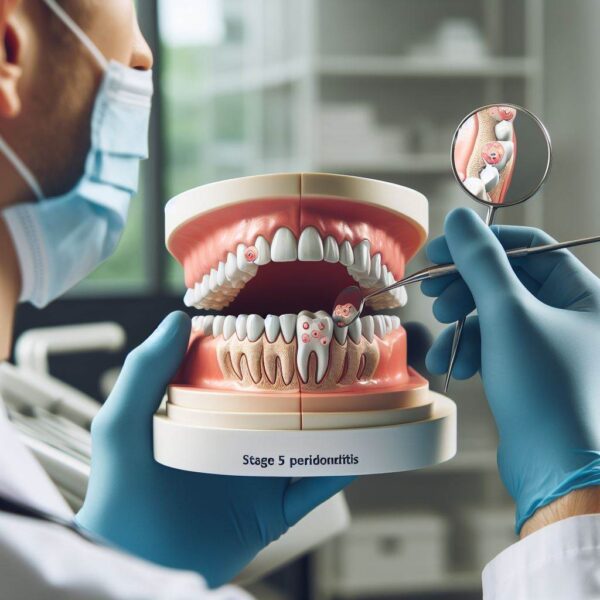
Stage V periodontitis, also known as advanced periodontitis, represents a critical stage in the progression of gum disease, characterized by severe damage to the supporting structures of the teeth.
As the most advanced form of periodontal disease, stage V periodontitis poses significant risks to oral health and overall well-being.
In this article, we delve into the complexities of stage V periodontitis, exploring its causes, symptoms, and potential treatment options to provide readers with valuable insights into this advanced dental condition.
Exploring Stage V Periodontitis:
Stage V periodontitis represents the pinnacle of gum disease progression, marked by extensive destruction of the bone and soft tissues that support the teeth. At this advanced stage, the gums may recede dramatically, exposing the roots of the teeth and leading to severe tooth mobility.
Deep pockets form between the teeth and gums, harboring harmful bacteria that perpetuate the cycle of infection and inflammation.
Causes of Stage V Periodontitis:
Multiple factors contribute to the development and progression of stage V periodontitis. Poor oral hygiene practices, including inadequate brushing and flossing, allow plaque and tartar to accumulate along the gumline, triggering inflammation and infection.
Smoking and tobacco use are significant risk factors for periodontal disease, as they compromise blood flow to the gums and impair the immune system’s ability to combat infections. Additionally, genetic predisposition, hormonal changes, and certain medical conditions, such as diabetes, can increase susceptibility to advanced gum disease.
What Is Stage 7 Periodontal Disease?
Stage VII periodontal disease, the most severe manifestation of gum disease, represents a critical juncture in oral health. Characterized by extensive damage to the supporting structures of the teeth, stage VII periodontal disease demands immediate attention and comprehensive treatment.
This advanced stage poses significant risks to oral health, including tooth loss and systemic health complications.
In this article, we delve into the complexities of stage VII periodontal disease, exploring its causes, symptoms, and potential treatment options to provide readers with valuable insights into this critical dental condition.
Exploring Stage VII Periodontal Disease:
Stage VII periodontal disease signifies the culmination of untreated or poorly managed gum disease, marked by profound destruction of the bone and soft tissues supporting the teeth. At this advanced stage, the gums may recede extensively, exposing the tooth roots and leading to severe tooth mobility.
Deep periodontal pockets form, harboring harmful bacteria that perpetuate infection and inflammation, exacerbating the condition.
Causes of Stage VII Periodontal Disease:
Multiple factors contribute to the development and progression of stage VII periodontal disease. Poor oral hygiene practices, such as inadequate brushing and flossing, allow plaque and tartar to accumulate along the gumline, triggering inflammation and infection.
Smoking and tobacco use significantly increase the risk of gum disease, as they compromise blood flow to the gums and weaken the immune system’s ability to combat infections.
Additionally, genetic predisposition, hormonal changes, and certain medical conditions, such as diabetes, can elevate susceptibility to advanced gum disease.
What Are The Different Stages Of Periodontitis?
Embarking on the journey of oral health, one encounters the multifaceted stages of periodontitis, a prevalent condition affecting millions globally. Understanding these distinct stages is paramount for effective management and treatment.
In this comprehensive article, we delve into the diverse phases of periodontitis, shedding light on their characteristics and implications to equip readers with the knowledge needed to safeguard their dental well-being effectively.
Exploring the Phases:
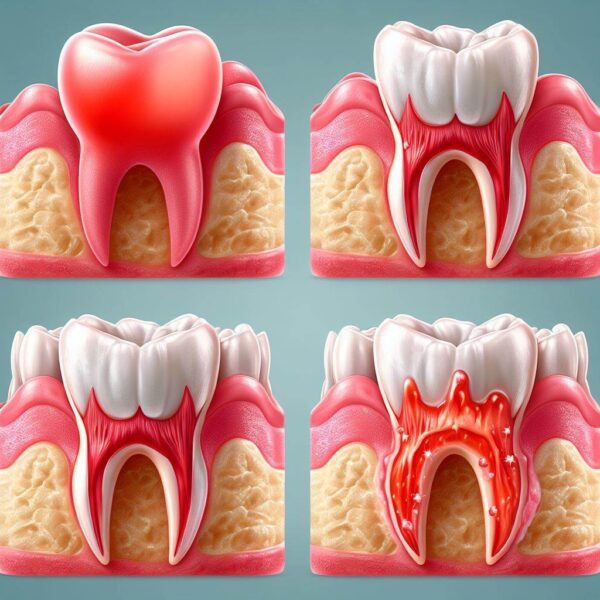
Phase One: Initial Onset – Gingivitis Transition
Gingivitis marks the initial stage of periodontitis, characterized by inflammation of the gums.
Symptoms include redness, swelling, and bleeding gums, often triggered by inadequate oral hygiene.
Gingivitis can progress to periodontitis without proper intervention, highlighting the importance of early detection and treatment.
Phase Two: Emerging Challenges – Early Periodontitis
Early periodontitis signifies the advancement of gingivitis, with deeper issues beginning to manifest.
Periodontal pockets form, allowing plaque and bacteria to accumulate below the gumline.
Symptoms escalate, including gum recession, tooth sensitivity, and persistent bad breath, indicating the need for intervention.
Phase Three: Advancement – Moderate Periodontitis
Moderate periodontitis denotes a significant escalation in tissue and bone damage.
Deepening of periodontal pockets exacerbates bone loss and compromises tooth stability.
Visible changes in tooth positioning and increased tooth mobility become evident, underscoring the urgency of treatment.
Phase Four: Critical Stage – Advanced Periodontitis
Advanced periodontitis represents the pinnacle of disease progression, with severe consequences for oral health.
Extensive destruction of bone and soft tissues leads to profound tooth mobility and eventual tooth loss.
Advanced periodontitis is associated with systemic conditions such as cardiovascular disease, highlighting the importance of comprehensive management.
Gingivitis Vs. Periodontitis
Gum disease is a common but often overlooked dental condition affecting millions of people worldwide. It typically begins as gingivitis and can progress to periodontitis if left untreated. Understanding the distinction between these two stages is crucial for effective prevention and treatment.
In this article, we will explore the key differences between gingivitis and periodontitis, shedding light on their unique characteristics, causes, symptoms, and treatment options. This knowledge is essential for maintaining optimal oral health and preventing serious complications.
Understanding Gingivitis:
Definition and Causes:
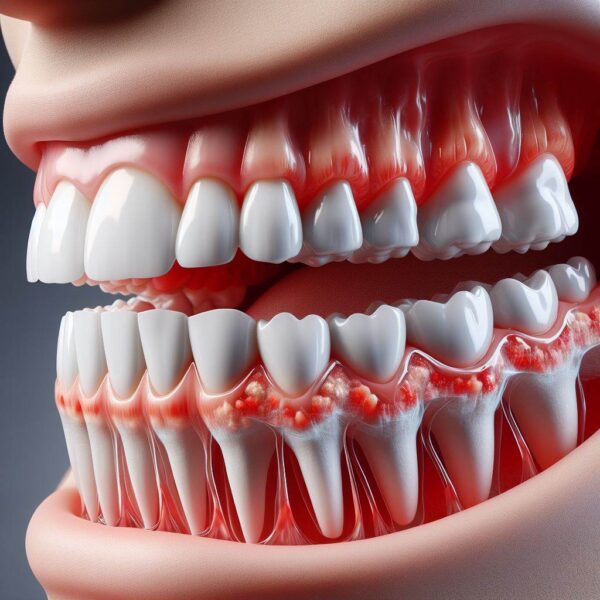
Gingivitis is the earliest stage of gum disease, characterized by inflammation of the gums.
It is primarily caused by the buildup of plaque, a sticky film of bacteria on the teeth.
Poor oral hygiene practices, such as inadequate brushing and flossing, contribute significantly to plaque accumulation.
Symptoms and Diagnosis:
Symptoms of gingivitis include red, swollen, and tender gums that may bleed during brushing or flossing.
Bad breath and receding gums can also be indicators of gingivitis.
A dentist diagnoses gingivitis through a clinical examination, noting the presence of plaque and inflammation.
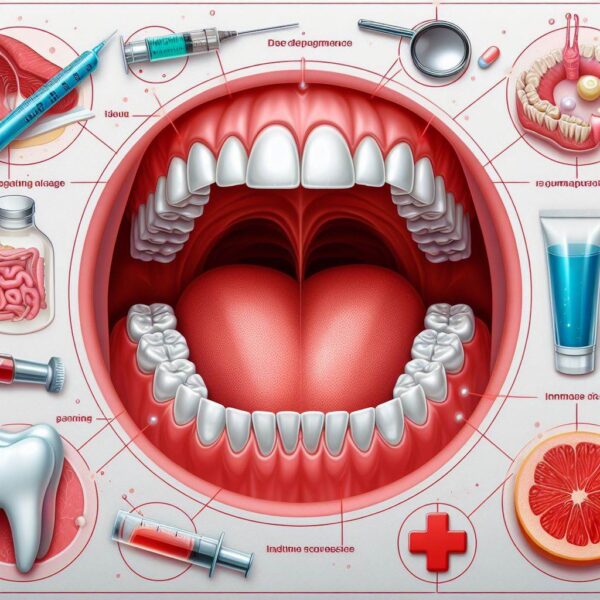
Treatment and Prevention:
Gingivitis is reversible with good oral hygiene practices, including regular brushing, flossing, and professional cleanings.
Antiseptic mouthwashes and improved dental care routines can help reduce plaque and inflammation.
Preventive measures include routine dental visits and maintaining a consistent oral hygiene regimen.
Understanding Periodontitis:
Definition and Causes:
Periodontitis is an advanced stage of gum disease that occurs when gingivitis is left untreated.
It involves the deeper structures of the gums and the supporting bone, leading to significant damage.
The progression from gingivitis to periodontitis is influenced by factors such as smoking, genetics, and systemic conditions like diabetes.
Symptoms and Diagnosis:
Symptoms of periodontitis are more severe and include persistent bad breath, loose teeth, and painful chewing.
Gum recession and the formation of deep periodontal pockets are common, resulting in tooth mobility and bone loss.
Diagnosis involves measuring the depth of periodontal pockets and assessing bone loss through dental X-rays.
Treatment and Management:
Treating periodontitis requires a more intensive approach, including scaling and root planing to remove plaque and tartar below the gumline.
Advanced cases may require surgical interventions, such as flap surgery or bone grafts, to restore damaged tissues.
Ongoing management involves regular dental check-ups, meticulous oral hygiene, and possibly the use of antibiotics to control infection.
Conclusion:
Periodontal disease is a progressive condition that, if left untreated, can lead to severe dental and systemic health issues. Recognizing the stages of periodontal disease—gingivitis, early periodontitis, moderate periodontitis, and advanced periodontitis—is crucial for timely intervention and effective treatment.
By maintaining good oral hygiene, scheduling regular dental check-ups, and addressing any signs of gum disease promptly, individuals can prevent the progression of periodontal disease and preserve their oral health.
Understanding these stages empowers patients to take proactive steps in safeguarding their smiles and overall well-being. I hope now you know everything about What Are The Stages Of Periodontal Disease.
FAQs:
Q1. What is the first stage of periodontal disease?
A: The first stage of periodontal disease is gingivitis. It is characterized by inflammation of the gums, which may appear red, swollen, and prone to bleeding during brushing or flossing. Gingivitis is primarily caused by plaque buildup and is reversible with good oral hygiene and professional dental care.
Q2. How does early periodontitis differ from gingivitis?
A: Early periodontitis occurs when gingivitis progresses and starts affecting the supporting bone and tissues around the teeth. This stage involves the formation of periodontal pockets, where plaque and bacteria accumulate below the gumline, leading to further inflammation and potential bone loss. Unlike gingivitis, early periodontitis requires more intensive treatment to halt its progression.
Q3. What are the symptoms of moderate periodontitis?
A: In moderate periodontitis, the damage extends deeper into the supporting bone and tissues. Symptoms include increased pocket depth between the gums and teeth, gum recession, tooth mobility, and possible changes in tooth positioning.
This stage often requires more aggressive cleaning procedures such as scaling and root planing to manage the condition.
Q4. What risks are associated with advanced periodontitis?
A: Advanced periodontitis is the most severe stage, marked by significant bone and tissue destruction. Risks include severe tooth mobility, tooth loss, and the potential spread of infection to other parts of the body. Advanced periodontitis is also linked to systemic health issues such as cardiovascular disease and diabetes. Treatment may involve surgical interventions to restore damaged tissues and maintain oral health.
Q5. Can periodontal disease be prevented?
A: Yes, periodontal disease can be prevented with diligent oral hygiene practices. This includes brushing twice daily, flossing regularly, and using antiseptic mouthwash. Regular dental check-ups and professional cleanings are essential to remove plaque and tartar buildup. Early detection and treatment of gingivitis can prevent its progression to more severe stages of periodontal disease.
