In the realm of healthcare, one must wonder Can I Take Tylenol Or Ibuprofen With Paxlovid & navigating the intricacies of medication interactions is a crucial aspect of managing one’s well-being. With the emergence of novel treatments like Paxlovid offering hope in the battle against COVID-19, questions naturally arise regarding its compatibility with other commonly used medications.
Among the inquiries frequently pondered by individuals seeking relief from symptoms or undergoing treatment is whether it’s safe to combine Paxlovid with over-the-counter pain relievers like Tylenol (acetaminophen) or Ibuprofen.
Can I Take Tylenol Or Ibuprofen With Paxlovid
Addressing this concern requires a balanced understanding of pharmacological principles, individual health factors, and expert guidance. As we delve into the topic of whether Tylenol or Ibuprofen can be safely taken alongside Paxlovid, it’s essential to approach it with clarity and discernment.
By examining the potential interactions, risks, and considerations involved, we can empower individuals to make informed decisions about their health and medication regimens.
Now, let’s delve into the details of combining Tylenol or Ibuprofen with Paxlovid, exploring key points to consider for a comprehensive understanding of this important issue.
1. Understanding Paxlovid:
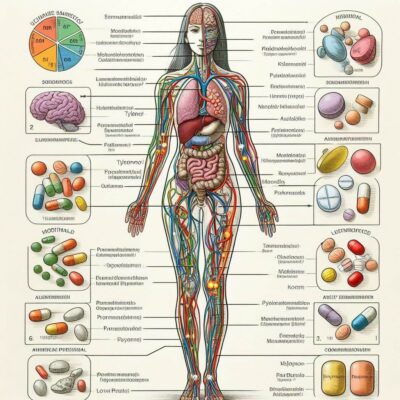
Before delving into potential interactions, it’s essential to grasp the nature of Paxlovid. This antiviral medication, recently authorized for emergency use, works by inhibiting the replication of the SARS-CoV-2 virus, the causative agent of COVID-19.
2. Mechanism of Action:
Tylenol and Ibuprofen, commonly used to alleviate pain and reduce fever, exert their effects through different mechanisms. Tylenol primarily functions as a pain reliever and fever reducer, while Ibuprofen possesses anti-inflammatory properties in addition to its analgesic and antipyretic effects.
3. Individual Considerations:
Despite the lack of direct interaction, individual health factors and medication histories must be taken into account. Patients with preexisting liver conditions, for example, may need to exercise caution when taking Tylenol due to its potential hepatotoxicity.
4. Expert Guidance:
Healthcare providers play a crucial role in guiding patients on medication use. Consulting a healthcare professional is advisable before combining Paxlovid with Tylenol or Ibuprofen, especially for individuals with underlying health conditions or those taking multiple medications.
5. Monitoring and Reporting:
Regular monitoring for adverse effects and open communication with healthcare providers are essential when using multiple medications concurrently. Any unusual symptoms or concerns should be promptly reported for further evaluation. I hope now you’re fully aware of Can I Take Tylenol Or Ibuprofen With Paxlovid?
What Is Paxlovid And Its Purpose?
In the ongoing battle against the COVID-19 pandemic, the search for effective treatments has been relentless. Amidst this quest, Paxlovid has emerged as a beacon of hope, offering a promising avenue in the fight against the novel coronavirus. But what exactly is Paxlovid, and what role does it play in the realm of COVID-19 therapeutics?
As the world grapples with the challenges posed by the pandemic, the urgency to develop effective antiviral medications has never been greater. Paxlovid, also known by its generic name nirmatrelvir/ritonavir, represents a significant advancement in this endeavor. Approved for emergency use authorization by regulatory agencies in several countries, including the FDA in the United States, Paxlovid holds the potential to change the landscape of COVID-19 treatment.
In this article, we’ll delve into the intricacies of Paxlovid, exploring its composition, mechanism of action, and therapeutic purpose. By gaining a deeper understanding of this innovative medication, we can shed light on its role in combating COVID-19 and its implications for public health efforts worldwide.
Paxlovid and Its Purpose:
1. Composition:
Paxlovid is a combination medication consisting of two active ingredients: nirmatrelvir and ritonavir. Nirmatrelvir is a potent inhibitor of the main protease of SARS-CoV-2, the virus responsible for COVID-19, while ritonavir is included to increase the plasma half-life of nirmatrelvir by inhibiting its metabolism.
2. Mechanism of Action:
Paxlovid exerts its antiviral effects by targeting the main protease enzyme essential for viral replication. By inhibiting this enzyme, Paxlovid interferes with the ability of the virus to replicate and spread within the body, thereby reducing the severity and duration of COVID-19 symptoms.
3. Therapeutic Purpose:
The primary purpose of Paxlovid is to treat mild to moderate cases of COVID-19 in non-hospitalized patients who are at high risk of progression to severe disease. By offering an oral treatment option that can be administered outside of hospital settings, Paxlovid aims to alleviate the burden on healthcare systems and provide patients with timely access to effective therapy.
4. Clinical Efficacy:
Clinical trials evaluating the efficacy of Paxlovid have shown promising results, demonstrating significant reductions in the risk of hospitalization and death among treated patients compared to those receiving placebo. These findings highlight the potential of Paxlovid to improve outcomes for individuals infected with SARS-CoV-2.
5. Regulatory Approval:
Paxlovid has received emergency use authorization from regulatory agencies in several countries, including the FDA in the United States. This authorization reflects the urgent need for effective COVID-19 treatments and the compelling evidence supporting the safety and efficacy of Paxlovid in clinical trials.
6. Administration and Availability:
Paxlovid is available in the form of oral tablets, making it convenient for patients to administer at home under medical supervision. The availability of Paxlovid represents a significant milestone in the global effort to combat COVID-19, offering a valuable addition to the arsenal of antiviral therapies available to healthcare providers.
Interaction Of Paxlovid With Tylenol
In the ever-evolving landscape of healthcare, the intersection of medications and their potential interactions is a topic of paramount importance. With the emergence of Paxlovid as a promising treatment for COVID-19, individuals and healthcare providers alike are keen to understand how this medication interacts with commonly used drugs. One such medication of interest is Tylenol (acetaminophen), a widely used over-the-counter pain reliever and fever reducer.
As patients seek clarity on whether Paxlovid can be safely combined with Tylenol, it’s essential to delve into the nuances of pharmacological interactions and individual health considerations. By examining the mechanisms of these medications and the potential implications of their concurrent use, we can provide valuable insights to guide informed decision-making in clinical practice.
In this article, we’ll explore the interaction of Paxlovid with Tylenol, shedding light on the factors at play and offering practical considerations for patients and healthcare providers alike.
Interaction:
1. Mechanism of Action:
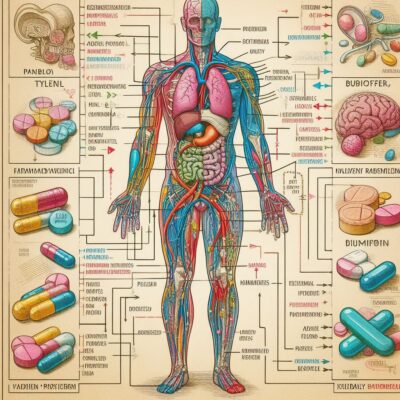
Paxlovid is an antiviral medication that works by inhibiting the main protease enzyme of SARS-CoV-2, the virus responsible for COVID-19. Tylenol, on the other hand, functions primarily as a pain reliever and fever reducer by inhibiting prostaglandin synthesis in the central nervous system.
2. Pharmacokinetic Interactions:
While both Paxlovid and Tylenol undergo metabolism in the liver, they are metabolized by different enzyme pathways. Paxlovid is primarily metabolized by the cytochrome P450 enzyme CYP3A4, while Tylenol is metabolized by various enzymes, including CYP2E1 and UDP-glucuronosyltransferases.
3. Potential Interactions:
Given that Paxlovid and Tylenol are metabolized by different enzyme pathways, there is generally no significant pharmacokinetic interaction between the two medications. This means that they can typically be used together without a significant increase in the risk of adverse effects or decreased efficacy.
4. Clinical Considerations:
While concurrent use of Paxlovid and Tylenol is generally considered safe, individual patient factors and medical history should be taken into account. Patients with preexisting liver conditions, for example, may need to exercise caution when using Tylenol due to its potential hepatotoxicity.
5. Monitoring and Reporting:
Healthcare providers should monitor patients closely for any signs of adverse effects or changes in medication efficacy when Paxlovid and Tylenol are used concomitantly. Patients should be advised to report any unusual symptoms or concerns to their healthcare provider promptly.
6. Expert Guidance:
As with any medication regimen, it’s essential for patients to consult with their healthcare provider before combining Paxlovid with Tylenol. Healthcare providers can offer personalized guidance based on individual health factors and medication histories to ensure safe and effective treatment.
Interaction Of Paxlovid With Ibuprofen
As the world continues to grapple with the challenges posed by the COVID-19 pandemic, the search for effective treatments remains a top priority. Among the emerging options is Paxlovid, a promising antiviral medication offering hope in the fight against the novel coronavirus.
With its potential to improve outcomes for individuals infected with COVID-19, questions naturally arise regarding its compatibility with other commonly used medications. One such medication of interest is Ibuprofen, a nonsteroidal anti-inflammatory drug (NSAID) widely used to alleviate pain and reduce inflammation.
Understanding the interaction between Paxlovid and Ibuprofen is essential for patients and healthcare providers alike. By exploring the pharmacological mechanisms at play and the potential implications of combining these medications, we can provide valuable insights to guide informed decision-making in clinical practice.
Interactions:
1. Mechanism of Action:
Paxlovid is an antiviral medication that works by inhibiting the main protease enzyme of SARS-CoV-2, the virus responsible for COVID-19. Ibuprofen, on the other hand, exerts its effects by inhibiting the enzymes cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2), thereby reducing inflammation, pain, and fever.
2. Pharmacokinetic Interactions:
Both Paxlovid and Ibuprofen undergo metabolism in the liver, albeit by different enzyme pathways. Paxlovid is primarily metabolized by the cytochrome P450 enzyme CYP3A4, while Ibuprofen is metabolized by the same enzyme pathway, albeit to a lesser extent.
3. Potential Interactions:
Given that Paxlovid and Ibuprofen are metabolized by overlapping enzyme pathways, there is a potential for pharmacokinetic interactions between the two medications. Specifically, coadministration of Paxlovid and Ibuprofen may result in increased plasma concentrations of Ibuprofen due to inhibition of its metabolism by Paxlovid.
4. Clinical Considerations:
The potential for pharmacokinetic interactions between Paxlovid and Ibuprofen underscores the importance of monitoring patients closely when these medications are used concomitantly. Healthcare providers should be vigilant for signs of Ibuprofen toxicity, such as gastrointestinal bleeding or renal impairment, and adjust the dosage of Ibuprofen as necessary.
5. Individual Patient Factors:
Individual patient factors, such as age, renal function, and concomitant medications, may influence the risk of adverse effects when Paxlovid and Ibuprofen are used together. Patients with preexisting renal impairment or a history of gastrointestinal bleeding, for example, may be at increased risk and require closer monitoring.
6. Expert Guidance:
As with any medication regimen, it’s essential for patients to consult with their healthcare provider before combining Paxlovid with Ibuprofen. Healthcare providers can offer personalized guidance based on individual health factors and medication histories to ensure safe and effective treatment.
Potential Interactions Of Paxlovid
As the COVID-19 pandemic continues to impact communities worldwide, the development of effective treatments remains a critical focus of medical research and practice. Paxlovid, a newly authorized antiviral medication, has emerged as a promising option in the fight against the novel coronavirus. However, as with any medication, understanding its potential interactions with other drugs is essential for ensuring safe and effective treatment regimens.
The concept of drug interactions encompasses a complex interplay of pharmacological mechanisms, metabolic pathways, and individual patient factors. With Paxlovid gaining traction as a frontline treatment for COVID-19, questions inevitably arise regarding its compatibility with commonly prescribed medications.
In this article, we’ll explore the potential interactions of Paxlovid, shedding light on the factors at play and providing insights to guide healthcare providers and patients in navigating the complexities of medication management.
Potential Interactions:
1. Pharmacokinetic Interactions:
Paxlovid undergoes metabolism primarily through the cytochrome P450 enzyme CYP3A4. As such, medications that inhibit or induce this enzyme may interact with Paxlovid, affecting its plasma concentration and efficacy.
2. CYP3A4 Inhibitors:
Drugs that inhibit CYP3A4, such as certain antifungal medications (e.g., ketoconazole, itraconazole) and HIV protease inhibitors (e.g., ritonavir), may increase the plasma concentration of Paxlovid, potentially leading to an increased risk of adverse effects.
3. CYP3A4 Inducers:
Conversely, drugs that induce CYP3A4 activity, such as rifampin (an antibiotic) and certain antiepileptic drugs (e.g., carbamazepine, phenytoin), may reduce the plasma concentration of Paxlovid, compromising its therapeutic efficacy.
4. QT Prolongation:
Paxlovid has been associated with QT interval prolongation, a potential risk factor for cardiac arrhythmias. Concurrent use of other medications known to prolong the QT interval, such as certain antibiotics (e.g., macrolides, fluoroquinolones) and antipsychotics (e.g., haloperidol, risperidone), may exacerbate this risk.
5. Renal Function:
Paxlovid is excreted primarily via the kidneys, and patients with impaired renal function may experience altered drug clearance and an increased risk of adverse effects. Healthcare providers should consider adjusting the dosage of Paxlovid in patients with renal impairment to minimize the risk of toxicity.
6. Hepatic Function:
Patients with preexisting liver conditions may also be at increased risk of adverse effects when taking Paxlovid, as hepatic metabolism plays a significant role in the clearance of the drug. Close monitoring of liver function tests is recommended in these patients to detect any signs of hepatotoxicity.
7. Individual Patient Factors:
Beyond pharmacokinetic considerations, individual patient factors such as age, comorbidities, and concomitant medications can influence the likelihood and severity of drug interactions with Paxlovid. Healthcare providers should conduct a thorough medication review and consider these factors when prescribing Paxlovid to optimize treatment outcomes and minimize risks.
8. Expert Guidance:
Given the complexity of drug interactions and the potential implications for patient safety and treatment efficacy, healthcare providers play a crucial role in guiding medication management. Consulting with a pharmacist or clinical pharmacologist can provide valuable insights and assistance in navigating potential interactions and optimizing treatment regimens.
Safety Considerations

In the realm of healthcare, safety considerations form the cornerstone of effective treatment strategies. Whether it’s prescribing medications, performing procedures, or implementing therapeutic interventions, ensuring the safety and well-being of patients is paramount. As new treatments emerge and medical practices evolve, maintaining a vigilant approach to safety remains essential to mitigate risks and optimize outcomes.
In this article, we’ll explore safety considerations in healthcare, focusing on the factors that contribute to patient safety, the importance of proactive risk management, and strategies for promoting a culture of safety in clinical settings. By examining these key aspects, we aim to highlight the significance of safety in healthcare delivery and empower healthcare providers and patients alike to prioritize safety in their interactions and decision-making processes.
Safety:
1. Patient-Centered Care:
At the heart of safety considerations in healthcare is a commitment to patient-centered care. This approach emphasizes the importance of engaging patients as active participants in their healthcare journey, fostering open communication, and respecting patients’ values, preferences, and autonomy.
2. Evidence-Based Practice:
Evidence-based practice forms the foundation of safe and effective healthcare delivery. By integrating the best available evidence from research, clinical expertise, and patient preferences, healthcare providers can make informed decisions that optimize patient outcomes while minimizing risks.
3. Medication Safety:
Medication safety is a critical aspect of patient care, given the widespread use of medications in healthcare. Healthcare providers must adhere to rigorous protocols for medication prescribing, dispensing, administration, and monitoring to prevent medication errors, adverse drug reactions, and other medication-related harms.
4. Infection Control:
Infection control practices play a vital role in preventing the spread of infectious diseases and ensuring the safety of patients, healthcare workers, and the community. Proper hand hygiene, use of personal protective equipment, adherence to standard precautions, and implementation of infection control protocols are essential for minimizing the risk of healthcare-associated infections.
5. Procedural Safety:
Safety considerations extend to procedural interventions, where attention to detail, adherence to protocols, and effective communication among healthcare team members are critical for preventing errors, complications, and adverse events. Implementing standardized procedures, conducting pre-procedure safety checks, and fostering a culture of teamwork and collaboration can enhance procedural safety.
6. Patient Safety Culture:
Promoting a culture of safety within healthcare organizations is essential for fostering a supportive environment where patient safety is prioritized, errors are openly reported and analyzed, and continuous improvement initiatives are embraced. Leadership commitment, staff engagement, and transparent communication are key drivers of a positive patient safety culture.
7. Quality Improvement:
Continuous quality improvement efforts are essential for identifying areas for improvement, implementing evidence-based interventions, and monitoring outcomes to enhance patient safety and healthcare quality. By engaging in systematic quality improvement initiatives, healthcare organizations can identify and address safety gaps, reduce errors, and optimize patient care delivery.
8. Health Information Technology:
Health information technology, including electronic health records (EHRs) and clinical decision support systems, can play a significant role in enhancing patient safety by facilitating accurate documentation, medication reconciliation, clinical decision-making, and communication among healthcare providers.
9. Patient Education and Empowerment:
Educating patients about their health conditions, treatment options, and self-care practices is crucial for empowering patients to actively participate in their healthcare and make informed decisions that promote their safety and well-being. Providing clear, understandable information, encouraging questions, and offering support resources can help patients take an active role in managing their health.
Pros And Cons Of Taking Tylenol Or Ibuprofen With Paxlovid?
Navigating the realm of medication interactions is a crucial aspect of managing one’s health, especially in the context of emerging treatments like Paxlovid for COVID-19. As individuals seek relief from symptoms and healthcare providers explore effective treatment options, questions naturally arise about the compatibility of Paxlovid with commonly used medications such as Tylenol (acetaminophen) and Ibuprofen.
Understanding the potential pros and cons of combining these medications is essential for making informed decisions about treatment regimens.
In this article, we’ll delve into the advantages and disadvantages of taking Tylenol or Ibuprofen alongside Paxlovid, exploring the benefits, risks, and considerations involved. By examining both sides of the equation, we aim to provide clarity and insights to empower individuals and healthcare providers in optimizing patient care and treatment outcomes.
Pros of Taking Tylenol or Ibuprofen with Paxlovid:
1. Symptom Management:
Tylenol and Ibuprofen can help alleviate symptoms such as pain and fever, which are common manifestations of COVID-19. By addressing these symptoms, they can improve patient comfort and quality of life.
2. Comprehensive Treatment:
Combining Tylenol or Ibuprofen with Paxlovid allows for a more comprehensive approach to managing COVID-19, targeting both viral replication and symptom relief simultaneously.
3. Flexibility in Treatment:
Offering options for pain relief gives patients flexibility in managing their symptoms, allowing them to tailor their treatment regimen to their individual needs and preferences.
Cons of Taking Tylenol or Ibuprofen with Paxlovid:
1. Potential for Drug Interactions:
Both Tylenol and Ibuprofen have their own potential for interactions with other medications. When combined with Paxlovid, there is a risk of pharmacokinetic interactions that could affect the metabolism and efficacy of either medication.
2. Increased Risk of Adverse Effects:
Taking multiple medications concurrently can increase the risk of adverse effects and complications, especially in vulnerable populations such as the elderly or those with preexisting medical conditions.
3. Complexity of Management:
Managing multiple medications adds complexity to treatment regimens, requiring careful monitoring, dosage adjustments, and coordination among healthcare providers to ensure safety and efficacy.
Considerations for Patient Safety:
1. Individual Health Factors:
Patient-specific factors such as age, underlying health conditions, and medication history should be taken into account when considering the use of Tylenol or Ibuprofen with Paxlovid.
2. Expert Guidance:
Healthcare providers play a crucial role in guiding treatment decisions and monitoring for potential interactions and adverse effects. Consulting with a healthcare professional is essential for ensuring safe and effective medication use.
3. Monitoring and Reporting:
Patients should be vigilant in monitoring for any signs of adverse effects or changes in symptoms and promptly report them to their healthcare provider for further evaluation.
Conclusion:
Navigating the realm of medication interactions requires careful consideration and informed decision-making. While seeking relief from symptoms and managing medical conditions, it’s essential to consult with healthcare providers and heed their advice to ensure safety and efficacy.
Whether it’s combining medications like Tylenol or Ibuprofen with Paxlovid or seeking guidance on broader healthcare concerns, the expertise of doctors serves as a valuable resource in promoting overall health and wellness. By fostering open communication, embracing preventive measures, and prioritizing patient-centered care, individuals can embark on a path toward better health with confidence and clarity. I hope now you understand Can I Take Tylenol Or Ibuprofen With Paxlovid.
FAQs:
Q1. Can I take Tylenol or Ibuprofen with Paxlovid?
A: While there is generally no direct contraindication to taking Tylenol or Ibuprofen alongside Paxlovid, it’s essential to consult with your healthcare provider before combining medications. They can assess your individual health factors, medication history, and potential risks to determine the safest and most effective treatment regimen for you.
Q2. What are the potential risks of combining Tylenol or Ibuprofen with Paxlovid?
A: Combining medications can increase the risk of adverse effects and drug interactions. Tylenol and Ibuprofen may have their own potential side effects, and concurrent use with Paxlovid could exacerbate these risks. Your healthcare provider can help weigh the potential benefits and risks and provide personalized guidance.
Q3. How should I monitor for adverse effects when taking Tylenol or Ibuprofen with Paxlovid?
A: It’s essential to monitor for any unusual symptoms or changes in your condition when taking multiple medications. Be vigilant for signs of adverse effects such as gastrointestinal discomfort, allergic reactions, or changes in liver or kidney function. If you experience any concerning symptoms, contact your healthcare provider promptly for further evaluation. “Can I Take Tylenol Or Ibuprofen With Paxlovid“
Q4. Are there any alternative medications or treatment options to consider instead of Tylenol or Ibuprofen with Paxlovid?
A: Depending on your specific health needs and the nature of your symptoms, your healthcare provider may recommend alternative medications or treatment approaches. They can discuss various options with you, taking into account factors such as medication interactions, potential side effects, and your treatment preferences. “Can I Take Tylenol Or Ibuprofen With Paxlovid“
Q5. What should I do if I have concerns or questions about taking Tylenol or Ibuprofen with Paxlovid?
A: If you have any concerns or questions about your medication regimen, don’t hesitate to reach out to your healthcare provider. They are there to address your concerns, provide guidance, and ensure that you receive safe and effective care. Open communication is key to optimizing your treatment outcomes and promoting your overall well-being. “Can I Take Tylenol Or Ibuprofen With Paxlovid“
