The presence of commensal flora in urine is a topic that may raise eyebrows and prompt questions about its significance and implications for health. Commensal flora refers to the diverse community of microorganisms that inhabit various parts of the human body, including the urinary tract.
While the urinary tract is traditionally considered a sterile environment, emerging research suggests that low levels of bacteria may be present in urine samples obtained from healthy individuals.
Understanding the presence of Commensal Flora Present In Urine What Does That Mean and its implications is crucial for healthcare professionals and individuals alike.
In this article, we’ll explore what it means to have commensal flora present in urine, the potential reasons behind its presence, and the implications for urinary tract health and clinical practice.
Commensal Flora Present In Urine What Does That Mean
The presence of commensal flora in urine samples may seem surprising, as the urinary tract has long been regarded as a sterile environment.
However, recent advancements in microbial detection techniques have challenged this notion, revealing that low levels of bacteria may indeed be present in urine samples obtained from healthy individuals. So, what does it mean to have commensal flora present in urine, and what are the implications?
1. Normal Microbiota of the Urinary Tract:
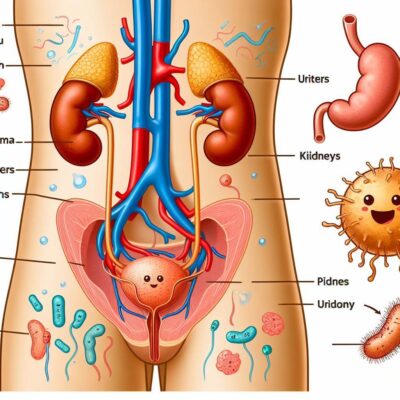
The urinary tract, including the bladder and urethra, is traditionally considered sterile in healthy individuals. However, emerging research suggests that the urinary tract harbors its own unique microbiota, consisting of a diverse community of bacteria, fungi, and other microorganisms.
This microbiota, often referred to as the urinary microbiome, plays a role in maintaining urinary tract health and function.
2. Low Levels of Bacteria in Urine:
Studies have demonstrated that low levels of bacteria may be present in urine samples obtained from healthy individuals, even in the absence of urinary tract infections (UTIs) or other urinary tract conditions.
These bacteria are often referred to as commensal or urotypes, and their presence does not necessarily indicate infection or pathology.
3. Potential Reasons for Presence:
The presence of commensal flora in urine samples may be attributed to various factors, including contamination during sample collection, transit of bacteria from the gastrointestinal tract or skin, colonization of the urinary tract by low-virulence bacteria, or host-microbiota interactions.
The composition and abundance of commensal flora in urine may vary among individuals and can be influenced by factors such as age, sex, hygiene practices, diet, and underlying health conditions.
4. Implications for Urinary Tract Health:
While the presence of commensal flora in urine samples obtained from healthy individuals may not necessarily indicate infection or pathology, it underscores the dynamic nature of the urinary microbiome and its potential role in urinary tract health and disease.
Disruptions to the urinary microbiome, such as alterations in microbial composition or dysbiosis, have been implicated in various urinary tract conditions, including UTIs, interstitial cystitis, and urinary incontinence.
5. Clinical Considerations:
The recognition of commensal flora in urine samples has important implications for clinical practice, particularly in the diagnosis and management of urinary tract conditions.
Healthcare professionals should exercise caution when interpreting urine culture results and consider factors such as patient demographics, symptoms, and medical history.
Summary Of Commensal Flora Present In Urine What Does That Mean:
The presence of commensal flora in urine samples obtained from healthy individuals challenges the traditional notion of urinary tract sterility and highlights the dynamic nature of the urinary microbiome.
While the implications of commensal flora in urine are still being elucidated, understanding its presence and significance is essential for advancing our knowledge of urinary tract health and disease.
Continued research in this area holds promise for improving the diagnosis, treatment, and prevention of urinary tract conditions and promoting overall urinary tract health. I hope now you are well aware of Commensal Flora Present In Urine What Does That Mean
Understanding Commensal Flora In Urine
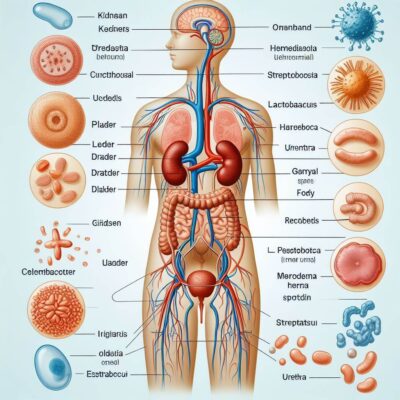
The human body is teeming with microorganisms, collectively known as the microbiota, which play crucial roles in maintaining health and supporting bodily functions. While the presence of bacteria in the gut and on the skin is well-known, less attention has been paid to the microbiota inhabiting the urinary tract.
Recent research has revealed that the urinary tract, traditionally considered sterile, also harbors its own unique microbial community, known as the urinary micro biota or commensal flora.
Understanding the composition and function of commensal flora in urine is an area of growing interest in the field of microbiology and urology. In this article, we’ll delve into the intricacies of commensal flora in urine, exploring its significance, implications for health, and emerging research in the field.
Understanding:
Commensal flora, also referred to as commensal microbiota, refers to the diverse community of microorganisms that inhabit various parts of the human body without causing harm to the host.
While the gut and skin microbiota have received considerable attention, the presence of commensal flora in the urinary tract has been less explored until recent years. Here’s what you need to know about commensal flora in urine:
1. Composition and Diversity:
The urinary tract, including the bladder and urethra, was traditionally believed to be sterile in healthy individuals. However, advancements in microbial detection techniques, such as next-generation sequencing and metagenomic analysis, have revealed that the urinary tract harbors its own microbial community.
The composition and diversity of commensal flora in urine vary among individuals and can be influenced by factors such as age, sex, hygiene practices, diet, and underlying health conditions.
2. Role in Urinary Tract Health:
The presence of commensal flora in urine may play a role in maintaining urinary tract health and function. These microorganisms may contribute to immune modulation, nutrient metabolism, and the prevention of pathogen colonization.
The urinary microbiota may also interact with the host epithelial cells and mucosal surfaces, influencing urinary tract homeostasis and defense mechanisms against infection.
3. Relationship to Urinary Tract Conditions:
Disruptions to the urinary microbiota, such as alterations in microbial composition or dysbiosis, have been implicated in various urinary tract conditions, including urinary tract infections (UTIs), interstitial cystitis, urinary incontinence, and kidney stones.
Changes in the urinary microbiota may predispose individuals to infections or exacerbate existing urinary tract conditions, highlighting the importance of maintaining a healthy microbial balance in the urinary tract.
4. Clinical Implications:
The recognition of commensal flora in urine samples has important implications for clinical practice, particularly in the diagnosis and management of urinary tract conditions.
Healthcare professionals should consider the presence of commensal flora when interpreting urine culture results and assessing urinary tract health. Further research is needed to elucidate the role of commensal flora in urinary tract health and disease and to develop targeted interventions for maintaining a healthy urinary microbiome.
5. Future Directions:
Continued research in the field of urinary microbiology holds promise for advancing our understanding of commensal flora in urine and its implications for health and disease.
Future studies may focus on characterizing the urinary microbiota in health and disease, elucidating its functional roles, exploring interactions with the host immune system, and developing microbiome-based therapies for urinary tract conditions.
Summary:
The presence of commensal flora in urine challenges the traditional notion of urinary tract sterility and underscores the importance of the urinary microbiota in maintaining urinary tract health and function.
Understanding the composition, function, and clinical implications of commensal flora in urine is essential for advancing our knowledge of urinary microbiology and developing strategies for promoting urinary tract health. I hope this helps you better understand Commensal Flora Present In Urine What Does That Mean
How Does Commensal Flora Colonize Urine?
The colonization of commensal flora in urine is a fascinating topic that sheds light on the dynamic relationship between the human body and its microbial inhabitants. While the urinary tract has long been considered a sterile environment, recent research has revealed that it is not immune to colonization by microorganisms.
Understanding how commensal flora colonize urine is essential for unraveling the complexities of the urinary microbiome and its implications for health and disease. In this article, we’ll delve into the mechanisms by which commensal flora colonize urine, exploring the factors that influence colonization, the role of host-microbe interactions, and the implications for urinary tract health.
Guide On Commensal Flora Colonize Urine:
The colonization of commensal flora in urine involves a complex interplay of factors, including microbial dynamics, host physiology, and environmental influences. Here’s a closer look at how commensal flora colonize urine:
1. Source of Colonization:
Commensal flora in urine can originate from various sources, including the gastrointestinal tract, skin, and external environment. Microorganisms from these sources can gain access to the urinary tract through ascending migration from the urethra or through hematogenous spread from distant sites in the body.
2. Urethral Colonization:
The urethra serves as a gateway for microbial colonization of the urinary tract. The periurethral area is home to a diverse community of microorganisms, including bacteria, fungi, and viruses, which can ascend into the bladder and other parts of the urinary tract.
Factors such as sexual activity, hygiene practices, and anatomical variations may influence the composition and abundance of microorganisms in the periurethral area and contribute to urethral colonization.
3. Bladder Colonization:
Once microorganisms gain access to the bladder, they may adhere to the bladder epithelium and form biofilms, complex microbial communities encased in a matrix of extracellular polymeric substances. Biofilm formation facilitates microbial persistence and resistance to host immune defenses and antimicrobial treatments.
Factors such as urinary stasis, urinary catheterization, and underlying bladder dysfunction may promote biofilm formation and bladder colonization.
4. Host-Microbe Interactions:
Host-microbe interactions play a crucial role in determining the outcome of microbial colonization in the urinary tract. The host immune system serves as the first line of defense against invading microorganisms, recognizing and responding to microbial antigens to prevent infection.
However, dysregulation of the immune response or alterations in the urinary microbiota may predispose individuals to urinary tract infections (UTIs) or other urinary tract conditions.
5. Environmental Influences:
Environmental factors, such as diet, lifestyle habits, medications, and exposure to antimicrobial agents, can influence microbial colonization in the urinary tract.
Changes in diet or medication use may alter the composition and abundance of commensal flora in urine, while exposure to antimicrobial agents may disrupt the urinary microbiota and promote the proliferation of pathogenic microorganisms.
6. Dynamic Nature of Colonization:
The colonization of commensal flora in urine is a dynamic process that can be influenced by various factors, including host immune responses, microbial competition, and environmental changes. The composition and abundance of commensal flora in urine may fluctuate over time in response to internal and external stimuli, highlighting the plasticity and adaptability of the urinary microbiome.
Role Of Commensal Flora In Maintaining Urinary Tract Health

The human body is home to trillions of microorganisms, collectively known as the microbiota, which play crucial roles in maintaining health and supporting bodily functions. While much attention has been focused on the gut microbiota, recent research has highlighted the importance of the microbiota inhabiting the urinary tract.
Among these microorganisms are commensal flora, which coexist with the host without causing harm. Understanding the role of commensal flora in maintaining urinary tract health is an area of growing interest in the field of urology and microbiology.
In this article, we’ll explore the role of commensal flora in maintaining urinary tract health, including their contributions to immune regulation, microbial balance, and defense against pathogens.
Role of Commensal Flora:
Commensal flora in the urinary tract play a vital role in maintaining urinary tract health through various mechanisms:
1. Immune Modulation:
Commensal flora interact with the host immune system to regulate immune responses and maintain immune homeostasis in the urinary tract. These microorganisms stimulate the production of anti-inflammatory cytokines and regulatory T cells, helping to prevent excessive immune activation and inflammation.
By modulating immune responses, commensal flora contribute to the maintenance of a balanced and tolerant immune environment in the urinary tract.
2. Microbial Balance:
Commensal flora help maintain microbial balance in the urinary tract by competing with potential pathogens for nutrients and colonization sites. By occupying niches within the urinary tract and producing antimicrobial substances, commensal flora inhibit the growth and proliferation of pathogenic microorganisms, preventing their overgrowth and colonization.
This competitive exclusion mechanism helps to maintain a diverse and stable microbial community in the urinary tract, which is essential for urinary tract health.
3. Biofilm Formation:
Commensal flora may form biofilms on the epithelial surfaces of the urinary tract, providing a protective barrier against invading pathogens and environmental insults.
Biofilms are complex microbial communities encased in a matrix of extracellular polymeric substances, which protect microorganisms from host immune defenses and antimicrobial treatments.
By forming biofilms, commensal flora helps maintain the integrity of the urinary tract mucosa and prevent colonization by pathogenic bacteria.
4. Metabolic Functions:
Commensal flora contributes to the metabolic functions of the urinary tract by metabolizing dietary components and host-derived molecules. These microorganisms produce short-chain fatty acids, vitamins, and other metabolites that support host nutrition and immune function.
By metabolizing urea and other nitrogenous compounds, commensal flora help regulate urinary pH and osmolality, maintaining optimal conditions for urinary tract health.
5. Prevention of Pathogen Colonization:
Commensal flora plays a critical role in preventing the colonization of the urinary tract by pathogenic microorganisms. By occupying available niches and competing with pathogens for resources, commensal flora limits the opportunity for pathogen establishment and proliferation.
Additionally, commensal flora produce antimicrobial substances, such as bacteriocins and hydrogen peroxide, which inhibit the growth of pathogenic bacteria and fungi.
Implications And Significance
Understanding the implications and significance of various phenomena is crucial for making informed decisions and advancing knowledge in any field. In the context of microbiology and health, recognizing the implications and significance of microbial interactions, processes, and findings can lead to improvements in diagnosis, treatment, and prevention strategies.
Let’s explore the implications and significance of a particular topic, providing insights into its importance and potential impact on health, research, and clinical practice.
Guide:
The implications and significance of a topic can have far-reaching effects on various aspects of human life, including health, research, and clinical practice. Here, we’ll delve into the implications and significance of a specific topic, examining its relevance and potential consequences:
1. Health Outcomes:
The implications of a topic on health outcomes are of paramount importance, as they directly impact the well-being of individuals and populations. Understanding the significance of certain microbial interactions or processes can lead to improved diagnostic methods, therapeutic interventions, and preventive measures to promote health and mitigate disease risks.
For example, identifying the role of specific commensal bacteria in maintaining gut health may inform dietary recommendations or probiotic therapies for managing gastrointestinal disorders.
2. Research Advancements:
The significance of a topic in research extends beyond immediate health outcomes, driving advancements in scientific knowledge and understanding. Investigating the implications of microbial phenomena can uncover new insights into disease mechanisms, host-microbe interactions, and therapeutic targets, leading to the development of innovative treatments and interventions.
By elucidating the significance of certain microbial processes, researchers can expand the frontiers of scientific inquiry and contribute to the collective body of knowledge in microbiology and related fields.
3. Clinical Practice:
In clinical practice, recognizing the implications of a topic can guide healthcare professionals in decision-making and patient management. Understanding the significance of certain microbial markers, diagnostic tests, or treatment modalities can improve clinical outcomes and patient care.
For example, recognizing the significance of antibiotic resistance patterns in urinary tract infections can inform antibiotic selection and prescribing practices, helping to optimize treatment efficacy and minimize the risk of resistance development.
4. Public Health Policies:
The implications of a topic may also influence public health policies and interventions aimed at promoting population health and preventing disease transmission. Recognizing the significance of certain microbial threats or risk factors can inform public health strategies for surveillance, control, and prevention.
For instance, understanding the implications of antimicrobial resistance in healthcare settings may lead to the implementation of infection control measures, antimicrobial stewardship programs, and public awareness campaigns to mitigate the spread of resistant pathogens.
5. Ethical Considerations:
Lastly, the implications of a topic may raise ethical considerations related to research conduct, patient care, and societal impact. Recognizing the significance of ethical principles such as beneficence, nonmaleficence, autonomy, and justice is essential for ensuring that research and clinical practices are conducted ethically and responsibly.
Addressing ethical implications associated with microbial research, such as informed consent, privacy protection, and equitable access to healthcare, is essential for upholding ethical standards and promoting societal well-being.
Relationship Between Commensal Flora And Urinary Tract Infections
The urinary tract, comprising the kidneys, ureters, bladder, and urethra, plays a crucial role in eliminating waste and maintaining fluid balance in the body. However, the urinary tract is not immune to microbial colonization and infection.
Urinary tract infections (UTIs) are among the most common bacterial infections, affecting millions of individuals worldwide each year. While pathogenic bacteria are often implicated in UTIs, recent research has highlighted the role of commensal flora in the urinary tract and its relationship to UTIs.
Understanding the complex interplay between commensal flora and urinary tract infections is essential for elucidating disease mechanisms, identifying risk factors, and developing targeted interventions. In this article, we’ll explore the relationship between commensal flora and urinary tract infections, examining how microbial dynamics, host factors, and environmental influences contribute to UTI pathogenesis and recurrence.
Detail Guide:
The relationship between commensal flora and urinary tract infections is multifaceted, involving microbial dynamics, host-microbe interactions, and environmental influences. Here’s a closer look at how commensal flora influence UTI pathogenesis and recurrence:
1. Microbial Dynamics:
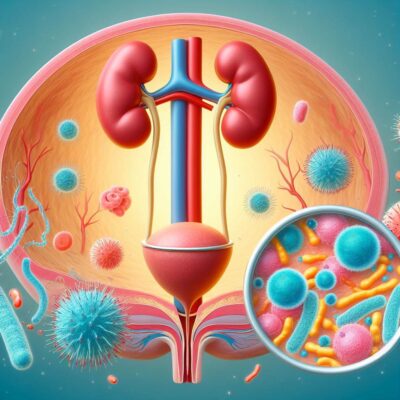
The urinary tract harbors its own unique microbial community, consisting of commensal flora as well as potential pathogens. Disruptions to the balance of commensal flora, such as alterations in microbial composition or dysbiosis, can create opportunities for pathogenic bacteria to colonize and infect the urinary tract.
Changes in the urinary microbiome may predispose individuals to UTIs by allowing pathogenic bacteria to outcompete commensal flora and establish infection.
2. Host-Microbe Interactions:
Commensal flora in the urinary tract play a critical role in maintaining host immune homeostasis and defending against pathogen colonization. These microorganisms interact with the host immune system to stimulate immune responses and prevent excessive inflammation.
However, dysregulation of host-microbe interactions or alterations in the urinary microbiome may compromise immune defenses and increase susceptibility to UTIs.
3. Environmental Influences:
Environmental factors, such as antibiotic use, urinary catheterization, sexual activity, and hormonal changes, can influence the composition and dynamics of commensal flora in the urinary tract, thereby affecting UTI risk.
Antibiotic therapy, while effective at treating UTIs, can disrupt the balance of commensal flora and promote the proliferation of antibiotic-resistant pathogens.
Urinary catheterization provides a direct route for microbial entry into the urinary tract, increasing the risk of catheter-associated UTIs. Hormonal changes, such as those occurring during pregnancy or menopause, may alter the urinary microbiome and predispose individuals to UTIs.
4. UTI Pathogenesis:
The pathogenesis of UTIs involves complex interactions between host factors, microbial virulence factors, and environmental conditions. Commensal flora may play a dual role in UTI pathogenesis, both protecting against and promoting infection.
Under normal circumstances, commensal flora compete with pathogenic bacteria for colonization sites and nutrients, limiting the opportunity for pathogen establishment.
However, disruptions to commensal flora or host immune defenses can tip the balance in favor of pathogen colonization, leading to UTI development.
5. UTI Recurrence:
Recurrent UTIs, defined as two or more episodes of infection within six months or three or more episodes within one year, are common among individuals with UTI history.
Commensal flora may influence UTI recurrence by modulating host immune responses, promoting microbial persistence, or altering the urinary microbiome. Factors such as antibiotic resistance, biofilm formation, and bladder dysfunction may contribute to recurrent UTIs by facilitating pathogen survival and reinfection.
Understanding the role of commensal flora in UTI recurrence is essential for developing targeted interventions to prevent recurrent infections and improve patient outcomes.
Managing Commensal Flora In Urine
The urinary tract, typically viewed as a sterile environment, is now known to harbor its own unique microbial community, known as commensal flora. These microorganisms, which include bacteria, fungi, and viruses, play essential roles in maintaining urinary tract health and function.
However, disruptions to the balance of commensal flora can lead to urinary tract infections (UTIs) and other urinary tract conditions. Managing commensal flora in urine is therefore crucial for promoting urinary tract health and preventing microbial imbalances.
Come let’s explore various strategies for managing commensal flora in urine, including dietary interventions, hygiene practices, probiotic supplementation, and antimicrobial therapies. By understanding how to maintain a healthy balance of commensal flora in the urinary tract, individuals can minimize the risk of UTIs and support overall urinary tract health.
Understand Commensal Flora in Urine:
Maintaining a healthy balance of commensal flora in the urinary tract is essential for preventing urinary tract infections and promoting urinary tract health. Here are some strategies for managing commensal flora in urine:
1. Dietary Interventions:
Diet plays a crucial role in shaping the composition and abundance of commensal flora in the urinary tract. Consuming a balanced diet rich in fiber, fruits, vegetables, and probiotic-rich foods can support the growth of beneficial microorganisms and help maintain a diverse and resilient urinary microbiome.
Avoiding excessive intake of sugary, processed, and high-fat foods may help prevent dysbiosis and microbial imbalances in the urinary tract.
2. Hygiene Practices:
Practicing good hygiene is essential for preventing the introduction and spread of pathogenic microorganisms in the urinary tract. Individuals should maintain proper genital hygiene, including regular cleansing of the genital area with mild soap and water.
Women should wipe from front to back after using the toilet to prevent the spread of fecal bacteria to the urinary tract. Additionally, individuals should avoid holding urine for prolonged periods and should empty their bladder completely during urination to minimize the risk of urinary stasis and bacterial overgrowth.
3. Probiotic Supplementation:
Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. Probiotic supplements containing strains of beneficial bacteria, such as Lactobacillus and Bifidobacterium, may help support a healthy urinary microbiome and prevent UTIs.
Studies have shown that probiotic supplementation can reduce the risk of recurrent UTIs by promoting the growth of beneficial bacteria and inhibiting the growth of pathogenic microorganisms in the urinary tract.
4. Antimicrobial Therapies:
In some cases, antimicrobial therapies may be necessary to manage commensal flora in urine, particularly in the context of UTIs or other urinary tract conditions. Antibiotics are commonly prescribed to treat bacterial UTIs and prevent complications such as kidney infection or sepsis.
However, indiscriminate use of antibiotics can disrupt the balance of commensal flora and promote the development of antibiotic-resistant bacteria. Therefore, antimicrobial therapies should be used judiciously and under the guidance of a healthcare professional to minimize the risk of adverse effects and antimicrobial resistance.
5. Lifestyle Modifications:
Making lifestyle modifications can also help manage commensal flora in urine and support urinary tract health. Maintaining a healthy weight, staying hydrated, and practicing stress-reduction techniques can help strengthen the immune system and promote overall well-being.
Additionally, avoiding tobacco use and limiting alcohol consumption can reduce inflammation and oxidative stress, which may contribute to urinary tract conditions.
How Do Normal Flora Affect Human Health?
Normal flora, also known as indigenous microbiota or microbiome, refers to the diverse community of microorganisms that inhabit various parts of the human body, including the skin, mouth, gastrointestinal tract, urinary tract, and reproductive organs.
While these microorganisms were once viewed solely as potential pathogens, it is now recognized that they play essential roles in maintaining human health and well-being. Normal flora contribute to numerous physiological processes, including digestion, immune regulation, and protection against pathogens.
Understanding how normal flora affect human health is crucial for appreciating the intricate relationship between microorganisms and the human body. In this article, we’ll explore the multifaceted ways in which normal flora influences human health, from supporting immune function to influencing mental well-being.
Guide On Normal Flora Affect Human Health:
The impact of normal flora on human health is far-reaching and multifaceted, encompassing various physiological systems and processes. Here’s a closer look at how normal flora affect human health:
1. Digestive Health:
Normal flora in the gastrointestinal tract plays a crucial role in digestion, nutrient absorption, and gut homeostasis. These microorganisms break down complex carbohydrates, ferment dietary fibers, and produce essential vitamins and metabolites that contribute to overall digestive health.
Additionally, normal flora helps maintain the integrity of the intestinal barrier and prevent the colonization of pathogenic bacteria, thus protecting against gastrointestinal infections and inflammatory bowel diseases.
2. Immune Regulation:
Normal flora interact with the host immune system to modulate immune responses and maintain immune homeostasis. These microorganisms stimulate the development and maturation of immune cells, such as T cells and regulatory T cells, which play key roles in immune surveillance and tolerance.
Normal flora also produce antimicrobial peptides and compete with pathogenic bacteria for colonization sites, helping to prevent infections and promote host defense mechanisms.
3. Metabolic Function:
Normal flora contribute to host metabolism by metabolizing dietary components and host-derived molecules. These microorganisms produce short-chain fatty acids, such as acetate, propionate, and butyrate, which serve as energy sources for colonocytes and have anti-inflammatory properties.
Additionally, normal flora regulate lipid metabolism, glucose homeostasis, and energy balance, influencing metabolic health and susceptibility to metabolic disorders such as obesity and diabetes.
4. Vitamin Production:
Normal flora in the gut synthesize essential vitamins, including vitamin K, B vitamins (such as biotin, folate, and cobalamin), and vitamin D. These vitamins play critical roles in various physiological processes, including blood coagulation, DNA synthesis, neurotransmitter production, and bone health.
The production of vitamin K by gut bacteria, for example, is essential for the synthesis of clotting factors in the liver and helps prevent bleeding disorders.
5. Protection Against Pathogens:
Normal flora provide colonization resistance against pathogenic bacteria by competing for nutrients and colonization sites, producing antimicrobial substances, and modulating host immune responses.
By occupying ecological niches within the human body, normal flora prevent the overgrowth and colonization of pathogenic bacteria, thus reducing the risk of infections and maintaining microbial balance.
Disruptions to the normal flora, such as antibiotic use or dietary changes, can compromise colonization resistance and increase susceptibility to infections.
6. Mental Health:
Emerging research suggests that the gut-brain axis, a bidirectional communication pathway between the gut and the brain, plays a role in mental health and cognitive function.
Normal flora in the gut produces neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA), which influence mood, behavior, and stress responses.
Alterations in the gut microbiota composition, known as dysbiosis, have been associated with psychiatric disorders such as depression, anxiety, and autism spectrum disorders.
7. Skin Health:
Normal flora on the skin, known as the skin microbiota, contribute to skin health by maintaining the acidic pH of the skin surface, producing antimicrobial peptides, and competing with pathogenic bacteria for colonization sites.
These microorganisms help prevent infections, regulate sebum production, and modulate the skin’s immune responses. Disruptions to the skin microbiota, such as excessive hygiene practices or exposure to environmental toxins, can disrupt skin barrier function and increase the risk of skin infections and inflammatory skin conditions.
Conclusion:
Understanding the presence and significance of commensal flora in urine is essential for appreciating the complex relationship between microorganisms and human health. While urine was traditionally considered sterile, recent research has revealed the existence of a diverse community of commensal bacteria inhabiting the urinary tract.
These microorganisms play crucial roles in maintaining urinary tract health, regulating immune responses, and protecting against pathogenic infections. By recognizing the importance of commensal flora in urine, healthcare professionals can develop strategies to promote microbial balance, prevent urinary tract infections, and improve patient outcomes.
Continued research in this field holds promise for advancing our understanding of urinary microbiology and developing targeted interventions to support urinary tract health. I hope you understand now fully Commensal Flora Present In Urine What Does That Mean.
FAQs:
Q1: What are commensal flora present in urine?
A: Commensal flora in urine refer to the diverse community of microorganisms, including bacteria, fungi, and viruses, that inhabit the urinary tract without causing harm to the host.
Q2: Why is it important to recognize commensal flora in urine?
A: Recognizing commensal flora in urine is important for understanding urinary tract health, immune regulation, and microbial balance. These microorganisms play essential roles in preventing pathogenic infections and maintaining urinary tract function.
Q3: How do commensal flora affect urinary tract health?
A: Commensal flora in urine contribute to urinary tract health by competing with pathogenic bacteria for colonization sites, stimulating immune responses, and maintaining microbial balance. Disruptions to commensal flora can increase the risk of urinary tract infections and other urinary tract conditions. “Commensal Flora Present In Urine What Does That Mean“
Q4: Can commensal flora in urine cause infections?
A: While commensal flora in urine generally do not cause infections, disruptions to microbial balance or host immune defenses can increase the risk of pathogenic infections. Proper management of commensal flora is essential for preventing urinary tract infections. “Commensal Flora Present In Urine What Does That Mean“
Q5: What can be done to support commensal flora in urine?
A: Supporting commensal flora in urine involves maintaining good hygiene practices, consuming a balanced diet rich in fiber and probiotics, staying hydrated, and avoiding unnecessary antimicrobial therapies. Probiotic supplementation may also help promote microbial balance in the urinary tract. “Commensal Flora Present In Urine What Does That Mean“
