Discovering a red patch in your mouth can be a cause for concern, prompting questions about its potential significance and implications for oral health. While not all red patches are indicative of cancer, they should not be ignored, as they could signify underlying issues that require attention.
Understanding the possible causes of red patches in the mouth, including the risk factors associated with oral cancer, is essential for early detection and timely intervention.
In this article, we’ll explore the significance of red patches in the mouth, potential causes, and steps individuals can take to address and monitor them effectively. By staying informed and proactive, individuals can prioritize their oral health and take appropriate action in response to concerning symptoms.
Mouth Cancer Red Patch
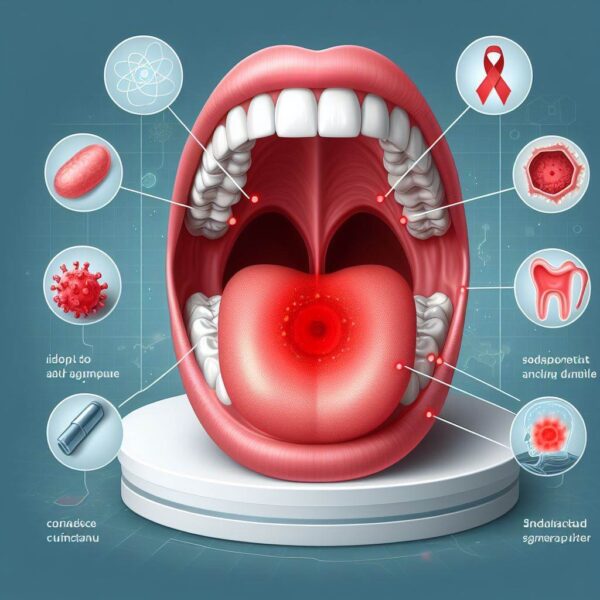
A red patch, also known as an erythroplakia, in the mouth can be a warning sign of various oral health issues, including oral cancer. While not all red patches are cancerous, they should be evaluated by a dentist or healthcare professional to determine their cause and appropriate treatment.
There are several potential causes of red patches in the mouth, ranging from benign conditions to more serious concerns. Common causes include irritation from dental appliances or rough foods, fungal infections such as oral thrush, autoimmune disorders like lichen planus, and allergic reactions to certain foods or medications.
However, one of the most concerning possibilities associated with red patches in the mouth is oral cancer. Oral cancer can manifest as red or white patches, ulcers, or lumps in the mouth or throat. Risk factors for oral cancer include tobacco use (both smoking and smokeless forms), excessive alcohol consumption, sun exposure to the lips, a diet low in fruits and vegetables, and infection with human papillomavirus (HPV).
Given the potential seriousness of oral cancer, it’s crucial not to ignore red patches or other unusual symptoms in the mouth. If you notice a persistent red patch or any other concerning symptoms such as pain, swelling, or difficulty swallowing, it’s essential to seek prompt evaluation by a dentist or healthcare professional. Early detection of oral cancer greatly improves the chances of successful treatment and recovery.
During a dental examination, your dentist will perform a thorough evaluation of your oral cavity, including the gums, tongue, cheeks, and throat. If a red patch or other abnormality is detected, your dentist may recommend further diagnostic tests such as a biopsy to determine the cause.
What Is Mouth Cancer Red Patch
Encountering a red patch in the mouth can be disconcerting, raising concerns about potential implications for oral health. While not all red patches indicate mouth cancer, they warrant attention as they might signal underlying issues necessitating evaluation.
Understanding the nature of a mouth cancer red patch, its distinctive features, and associated risk factors is crucial for early detection and management. In this article, we’ll explore the significance of mouth cancer red patches, examining their appearance, possible causes, and proactive measures individuals can take to address them effectively.
By staying informed and proactive, individuals can prioritize their oral health and take appropriate steps in response to concerning symptoms.
Exploring The Significance Of Mouth Cancer Red Patches:
1. Appearance:
A mouth cancer red patch presents as a flat or slightly raised area of red or velvety tissue in the oral cavity, often exhibiting a tendency to bleed easily when disturbed.
2. Distinctive Features:
Characteristics that may differentiate a mouth cancer red patch from benign conditions include persistent redness, irregular borders, a velvety texture, and a propensity to bleed upon manipulation.
3. Potential Causes:
Contributing factors to the development of mouth cancer red patches include chronic irritation from tobacco use, excessive alcohol consumption, sun exposure to the lips, a diet lacking in fruits and vegetables, HPV infection, and compromised immune function.
4. Risk Factors:
Individuals with a history of tobacco or alcohol use, sun exposure, poor diet, HPV infection, or weakened immune systems are at an increased risk of developing mouth cancer red patches.
5. Evaluation and Diagnosis:
It’s essential for individuals noticing suspicious red patches in their mouths to seek evaluation by a dentist or healthcare professional. A thorough examination, including visual inspection and potentially biopsy, may be necessary to determine the cause of the red patch.
6. Early Detection:
Early detection of mouth cancer red patches is critical for favorable treatment outcomes. Prompt evaluation and intervention increase the likelihood of successful management and recovery.
7. Treatment:
Treatment for mouth cancer red patches may involve surgical removal, radiation therapy, chemotherapy, or a combination of these modalities, depending on the extent and severity of the condition.
8. Preventive Measures:
Adopting preventive measures such as avoiding tobacco and excessive alcohol consumption, practicing sun safety, maintaining a balanced diet rich in fruits and vegetables, and receiving the HPV vaccine can help reduce the risk of developing mouth cancer red patches.
9. Regular Monitoring:
Individuals with a history of mouth cancer red patches should undergo regular follow-up appointments with their healthcare providers to monitor for recurrence or new lesions and ensure timely intervention if needed.
10. Overall Well-being:
Prioritizing oral health through proactive measures such as regular dental check-ups, proper oral hygiene practices, and avoidance of known risk factors contributes to overall well-being and reduces the likelihood of developing mouth cancer red patches.
What Does Mouth Cancer Patch Look Like?
Discovering a patch in the mouth that appears different from surrounding tissue can raise concerns about oral health, prompting questions about its potential significance. While not all patches in the mouth are indicative of mouth cancer, it’s essential to recognize the characteristics of a mouth cancer patch to ensure timely evaluation and intervention.
Understanding what a mouth cancer patch looks like, its distinguishing features and associated risk factors is crucial for early detection and management. In this article, we’ll explore the appearance of mouth cancer patches, describe their visual characteristics, and discuss proactive measures individuals can take in response to concerning symptoms.
By staying informed and proactive, individuals can prioritize their oral health and take appropriate action to address suspicious patches in the mouth.
The Appearance Of Mouth Cancer Patches:
1. Irregular Shape:
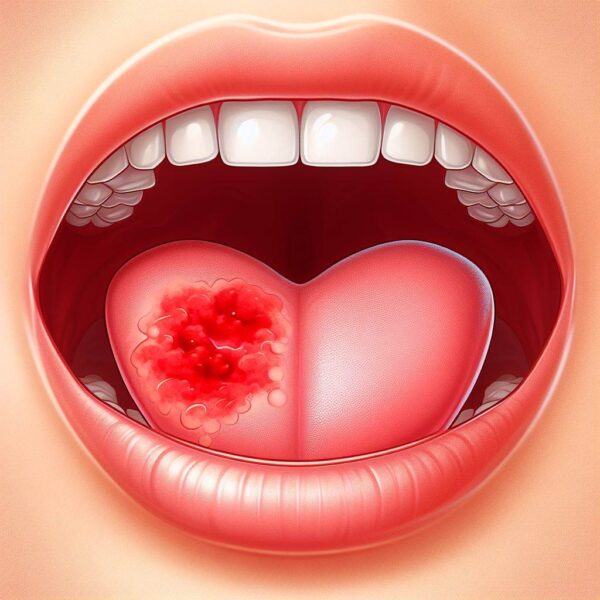
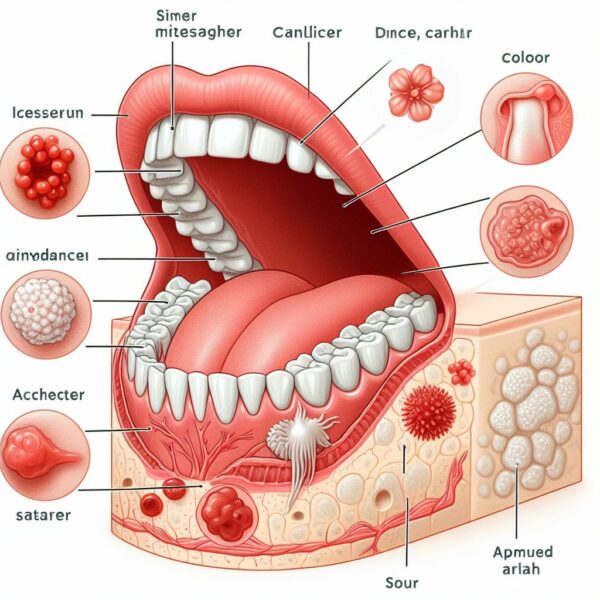
Mouth cancer patches often have irregular shapes, with jagged or undefined borders that may blend into the surrounding tissue.
2. Changes in Color:
These patches may appear red, white, or a combination of both, with variations in hue and intensity compared to adjacent tissues.
3. Textural Differences:
Mouth cancer patches may exhibit changes in texture, appearing rough, velvety, or thickened compared to the normal mucosa.
4. Persistent Presence:
Unlike temporary irritations or injuries that resolve on their own, mouth cancer patches tend to persist for weeks or months without significant improvement.
5. Ulceration or Bleeding:
Some mouth cancer patches may develop into ulcers or sores that do not heal, or they may bleed easily when touched or disturbed.
6. Location:
Mouth cancer patches can occur anywhere in the oral cavity, including the lips, tongue, cheeks, gums, palate, or throat.
7. Associated Symptoms:
In addition to visual changes, individuals with mouth cancer patches may experience symptoms such as pain, discomfort, difficulty swallowing, or changes in taste.
8. Risk Factors:
Factors that increase the risk of developing mouth cancer patches include tobacco use (smoking or chewing), excessive alcohol consumption, sun exposure to the lips, HPV infection, and a weakened immune system.
9. Evaluation and Diagnosis:
If a suspicious patch is identified in the mouth, it’s essential to seek evaluation by a dentist or healthcare professional. Diagnostic procedures such as visual inspection, biopsy, or imaging studies may be necessary to confirm the diagnosis.
10. Treatment and Management:
Treatment for mouth cancer patches typically involves surgical removal of the affected tissue, followed by radiation therapy, chemotherapy, or targeted therapy as needed. Early detection and intervention improve the chances of successful treatment outcomes.
What Are The Safety Measures to Take After Having Red Patch

After discovering a red patch in the mouth, it’s natural to feel concerned about its potential implications for oral health. While not all red patches indicate serious issues, taking appropriate safety measures is essential to ensure proper evaluation and management.
Understanding the safety measures to take after encountering a red patch can help individuals navigate the next steps effectively and prioritize their oral health.
In this article, we’ll explore the safety measures individuals should consider after noticing a red patch in the mouth, including seeking professional evaluation, practicing good oral hygiene, monitoring for changes, and addressing any associated symptoms.
By staying informed and proactive, individuals can take control of their oral health and address red patches in the mouth in a timely and effective manner.
Safety Measures Individuals Should Consider:
1. Practice Good Oral Hygiene:
Maintain good oral hygiene practices, including brushing your teeth at least twice a day with fluoride toothpaste and flossing daily to remove plaque and bacteria from between teeth and along the gum line.
2. Avoid Irritants:
Avoid any potential irritants that may exacerbate the red patch, such as tobacco use, excessive alcohol consumption, spicy or acidic foods, and rough or abrasive dental hygiene products.
3. Monitor for Changes:
Monitor the red patch for any changes in size, color, texture, or associated symptoms such as pain, discomfort, or difficulty swallowing. If you notice any concerning changes, contact your healthcare provider promptly.
4. Manage Discomfort:
If the red patch is causing discomfort or pain, consider using over-the-counter pain relievers or topical oral pain relief products as directed by your healthcare provider.
5. Stay Hydrated:
Drink plenty of water to stay hydrated and promote oral health. Hydration is essential for maintaining healthy oral tissues and facilitating healing.
6. Eat a Balanced Diet:
Maintain a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to support overall health and immune function. Nutritious foods can help promote healing and reduce the risk of complications.
7. Avoid Self-Diagnosis:
Avoid attempting to self-diagnose the red patch or seeking treatment without professional guidance. Only a healthcare professional can provide an accurate diagnosis and appropriate treatment plan.
8. Stay Informed:
Stay informed about oral health issues and seek guidance from reputable sources to ensure you’re taking the necessary safety measures to address the red patch effectively.
9. Follow Recommendations:
Follow any recommendations provided by the healthcare professional, which may include further diagnostic tests such as a biopsy to confirm the diagnosis.
Conclusion:
Being aware of the potential signs of mouth cancer, such as red patches in the mouth, is crucial for maintaining oral health and overall well-being. While not all red patches indicate cancer, they should not be ignored, as they could signify underlying issues requiring evaluation and management.
Seeking prompt professional evaluation and taking appropriate action can significantly improve treatment outcomes and prognosis. By staying informed, proactive, and vigilant about oral health, individuals can prioritize early detection and intervention, reducing the impact of mouth cancer and promoting a healthier future. I hope now you know everything about Mouth Cancer Red Patch and how to keep yourself safe from it.
FAQs:
Q1: What causes red patches in the mouth?
A: Red patches in the mouth can be caused by various factors, including irritation from dental appliances, fungal infections, autoimmune disorders, allergic reactions, or potentially more serious conditions such as oral cancer.
Q2: How do I know if a red patch in my mouth is cancerous?
A: While not all red patches are cancerous, characteristics that may raise suspicion include persistent redness, irregular borders, a velvety texture, a tendency to bleed easily, and associated symptoms such as pain or discomfort. It’s essential to seek evaluation by a dentist or healthcare professional for proper diagnosis and management.
Q3: What are the risk factors for developing mouth cancer red patches?
A: Risk factors for developing mouth cancer red patches include tobacco use (smoking or chewing), excessive alcohol consumption, sun exposure to the lips, HPV infection, and a weakened immune system.
Q4: Can red patches in the mouth be treated?
A: Treatment for red patches in the mouth depends on the underlying cause. If caused by benign conditions, such as irritation or infection, treatment may involve addressing the underlying issue with medications or lifestyle changes. If suspicious of cancer, treatment may involve surgical removal, radiation therapy, chemotherapy, or a combination of these modalities.
Q5: What should I do if I notice a red patch in my mouth?
A: If you notice a red patch in your mouth that persists for more than two weeks, seek evaluation by a dentist or healthcare professional. They can perform a thorough examination, including visual inspection and potentially biopsy, to determine the cause and appropriate treatment plan. Early detection and intervention are crucial for favorable treatment outcomes.
