Oral cancer is a serious health concern that affects thousands of individuals each year. Despite advancements in medical science, the mortality rate for oral cancer remains high, largely due to late-stage diagnosis.
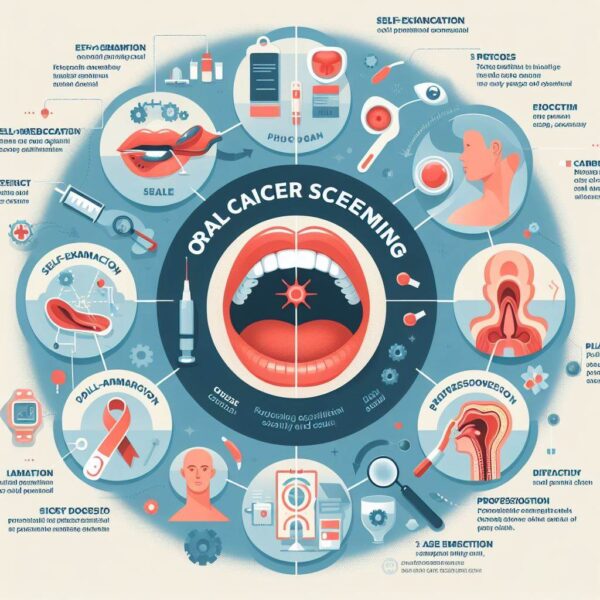
However, early detection through regular screening can significantly improve prognosis and treatment outcomes. Oral cancer screening is a proactive measure aimed at identifying signs of oral cancer or precancerous conditions in their earliest stages when they are most treatable.
By raising awareness about the importance of oral cancer screening and providing insights into the screening process, this article aims to empower individuals to prioritize their oral health and seek timely medical intervention when needed.
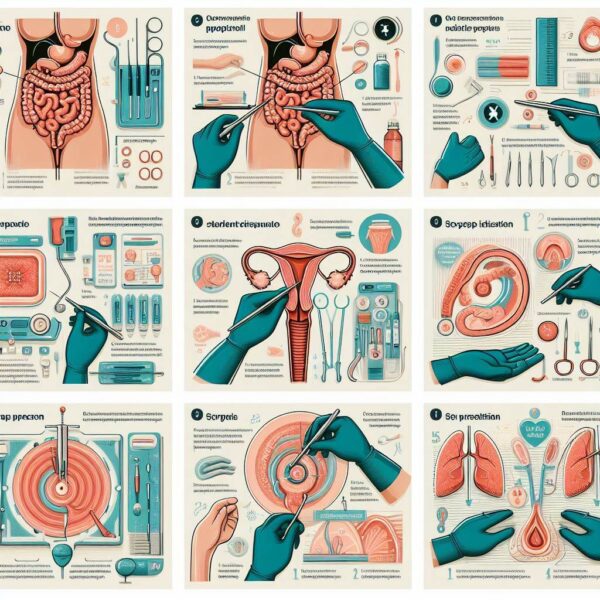
Screening For Oral Cancer
Oral cancer screening is a crucial aspect of preventive healthcare, particularly for individuals with known risk factors or those presenting with suspicious symptoms. Here’s what you need to know about oral cancer screening:
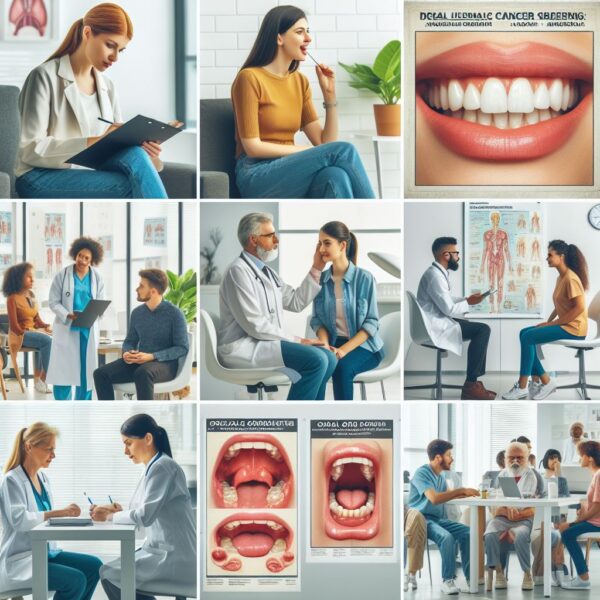
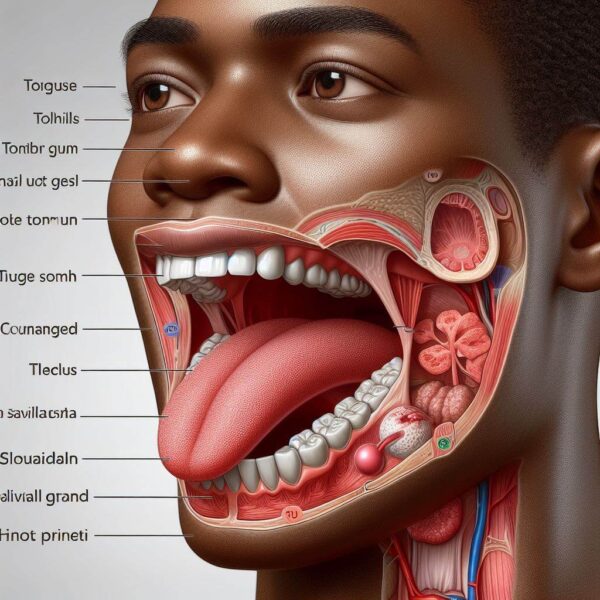
Oral cancer screening is typically performed during routine dental check-ups or medical examinations. Healthcare professionals, including dentists, oral surgeons, and primary care physicians, conduct visual inspections of the mouth, lips, tongue, gums, palate, and throat to detect any abnormalities that may indicate the presence of oral cancer or pre-cancerous lesions.
During the screening process, healthcare providers look for signs such as unusual lumps, bumps, sores, patches, or changes in the color or texture of the oral tissues. Additionally, they may inquire about the patient’s medical history, lifestyle habits (e.g., tobacco use, alcohol consumption), and any symptoms or concerns related to oral health.
In some cases, healthcare providers may use additional diagnostic tools or tests to aid in the detection of oral cancer. These may include oral brush biopsies, toluidine blue staining, fluorescence imaging, or other imaging modalities such as X-rays or CT scans.
The frequency of oral cancer screening depends on individual risk factors and recommendations from healthcare providers. Generally, individuals at higher risk, such as tobacco users, heavy drinkers, or those with a history of oral cancer, may require more frequent screenings, typically once a year or as recommended by their healthcare provider.
Early detection of oral cancer is critical for improving treatment outcomes and increasing survival rates. By identifying suspicious lesions or abnormalities early, healthcare professionals can initiate prompt medical intervention, potentially saving lives and preserving oral function and quality of life. I hope by reading this article you understand about Screening For Oral Cancer.
Understanding Screening For Oral Cancer
Oral cancer stands as a formidable adversary in the realm of healthcare, affecting individuals across the globe with its potentially devastating consequences. Despite medical advancements, late-stage diagnosis remains a prevalent issue, significantly impacting treatment efficacy and patient outcomes.
Yet, amidst this challenge lies a beacon of hope: early detection through regular screening. Understanding the significance and nuances of oral cancer screening is paramount for individuals to proactively safeguard their oral health. This article aims to unravel the complexities surrounding oral cancer screening, elucidating its importance, methodologies, and implications.
By shedding light on this critical aspect of preventive healthcare, we endeavor to empower individuals to take charge of their well-being and embrace the proactive measures available for early detection and intervention.
Defining Oral Cancer Screening:
Oral cancer screening entails a systematic examination of the oral cavity by healthcare professionals to identify any signs or symptoms indicative of oral cancer or pre-cancerous lesions.
• Importance of Early Detection:
Early detection through screening significantly enhances treatment outcomes and survival rates by enabling timely intervention and management of oral cancer.
• Screening Process:
During an oral cancer screening, healthcare providers visually inspect the oral tissues for abnormalities, including lumps, sores, lesions, discolorations, or changes in texture.
• Diagnostic Tools and Techniques:
In addition to visual examination, healthcare professionals may utilize diagnostic aids such as oral brush biopsies, toluidine blue staining, fluorescence imaging, or imaging modalities like X-rays or CT scans to aid in the detection of oral cancer.
• Frequency of Screening:
The frequency of oral cancer screening depends on individual risk factors and healthcare provider recommendations. Generally, individuals at higher risk may require more frequent screenings, typically annually or as advised by their healthcare provider.
• Empowering Individuals:
By understanding the significance of oral cancer screening and actively participating in regular screenings, individuals can take proactive steps toward safeguarding their oral health and well-being.
Epidemiology Of Screening Oral Cancer
Oral cancer represents a significant public health concern globally, with its prevalence and incidence rates varying across regions and populations. While advancements in screening methodologies have contributed to early detection and improved outcomes, challenges persist in reaching at-risk individuals and ensuring equitable access to screening services.
Understanding the epidemiology of screening for oral cancer is paramount in addressing disparities, enhancing screening effectiveness, and ultimately reducing the burden of this disease.
In this article, we delve into the complex landscape of oral cancer screening epidemiology, exploring factors influencing screening uptake, disparities in access and utilization, and strategies to optimize screening efforts for maximal impact.
Global Burden of Oral Cancer:
Oral cancer ranks among the top 10 most common cancers worldwide, with an estimated annual incidence of over 350,000 cases. The burden of oral cancer varies geographically, with higher incidence rates reported in South Asia, Southeast Asia, and parts of Central and Eastern Europe.
1. Vulnerable Populations:
Certain populations, such as older adults, men, individuals with low socioeconomic status, and those from marginalized communities, are disproportionately affected by oral cancer and may face barriers to accessing screening services.
2. Role of Screening in Early Detection:
Oral cancer screening plays a crucial role in detecting abnormalities in the oral cavity at early stages when treatment is most effective. Regular screening can facilitate early diagnosis, prompt intervention, and improved patient outcomes.
3. Screening Modalities and Techniques:
Screening for oral cancer primarily involves visual inspection of the oral cavity by healthcare professionals. In addition to visual examination, adjunctive diagnostic tools such as toluidine blue staining, oral brush biopsies, fluorescence imaging, and imaging modalities like X-rays or CT scans may be employed to aid in the detection of suspicious lesions.
4. Challenges and Disparities in Screening Uptake:
Despite the importance of oral cancer screening, disparities exist in screening uptake and access to services. Barriers to screening include lack of awareness, financial constraints, limited access to healthcare facilities, cultural beliefs, and language barriers, particularly among underserved and marginalized populations.
5. Strategies to Enhance Screening Efforts:
Addressing disparities in oral cancer screening requires multifaceted approaches, including targeted educational campaigns, community outreach programs, collaboration with community health workers, integration of screening services into primary care settings, and leveraging technology for telehealth and mobile screening initiatives.
6. Future Directions and Public Health Implications:
Optimizing oral cancer screening efforts necessitates a comprehensive understanding of epidemiological trends, risk factors, and barriers to screening uptake. By implementing evidence-based strategies and promoting equity in screening access, healthcare systems can mitigate the burden of oral cancer and improve outcomes for at-risk populations.
Risk Factors For Oral Cancer
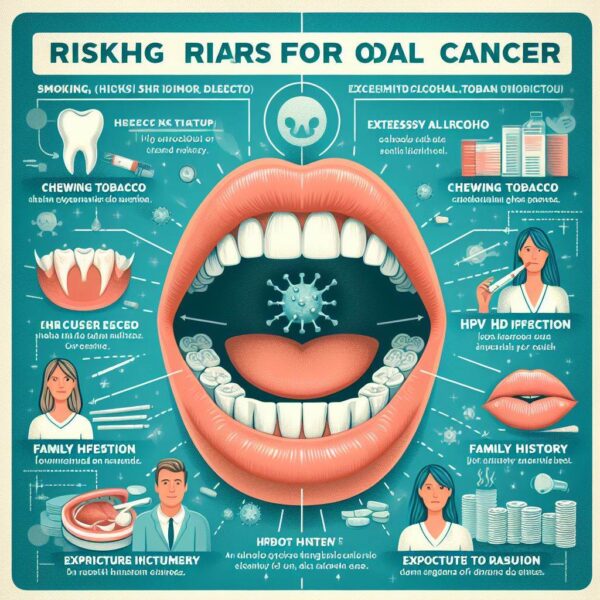
Oral cancer continues to pose a significant health challenge worldwide, with its incidence rates influenced by a myriad of factors, both behavioral and environmental. Understanding the risk factors associated with oral cancer is crucial for early detection, prevention, and effective management of this disease.
In this article, we delve into the multifaceted landscape of risk factors for oral cancer, ranging from lifestyle habits to genetic predispositions. By shedding light on these factors, we aim to raise awareness and empower individuals to take proactive measures to reduce their risk of developing oral cancer.
Exploring The Risk Factors:
1. Tobacco Use:
Tobacco use, including smoking cigarettes, cigars, pipes, and chewing tobacco, is one of the most significant risk factors for oral cancer. The carcinogenic compounds present in tobacco products can damage the cells lining the oral cavity, increasing the likelihood of cancer development.
2. Alcohol Consumption:
Heavy alcohol consumption is strongly associated with an increased risk of oral cancer. Alcohol can irritate the oral tissues and interact with carcinogens in tobacco, further elevating the risk of cancer development. The risk is particularly heightened in individuals who both smoke and drink alcohol excessively.
3. Betel Quid Chewing:
Betel quid, a mixture of betel leaf, areca nut, and slaked lime, is commonly chewed in many parts of Asia and the Pacific. The habit of betel quid chewing is strongly linked to oral cancer, with the carcinogenic substances present in areca nut and tobacco contributing to cancer development.
4. HPV Infection:
Certain strains of the human papillomavirus (HPV), particularly HPV-16 and HPV-18, have been implicated in the development of oral cancer. HPV-related oral cancers tend to affect the oropharynx and are more prevalent among younger individuals.
5. Poor Oral Hygiene:
Inadequate oral hygiene practices, including infrequent brushing and flossing, can lead to the accumulation of plaque and bacteria in the oral cavity. Chronic inflammation and irritation of the oral tissues increase the risk of oral cancer development over time.
6. Dietary Factors:
Poor dietary habits, such as a diet low in fruits and vegetables and high in processed foods and red meat, have been associated with an increased risk of oral cancer. Consuming a balanced diet rich in antioxidants and nutrients can help reduce the risk of cancer development.
7. Genetic Predisposition:
Genetic factors may influence an individual’s susceptibility to oral cancer. A family history of oral cancer or certain genetic mutations may increase the likelihood of developing the disease, although the precise mechanisms are still being investigated.
8. Sun Exposure:
Prolonged exposure to ultraviolet (UV) radiation from the sun can increase the risk of lip cancer. Outdoor workers and individuals with fair skin are particularly susceptible to lip cancer due to sun exposure.
Factors That Delay Cancer Detection In Primary Settings
Early detection is paramount in the successful treatment of cancer, yet delays in diagnosis remain a persistent challenge in primary healthcare settings. Identifying the factors contributing to these delays is crucial for implementing effective interventions and improving patient outcomes.
In this article, we delve into the complex web of reasons behind delayed cancer detection in primary care settings. By understanding these factors, healthcare providers and policymakers can work towards streamlining diagnostic processes, enhancing patient education, and optimizing healthcare delivery to ensure timely cancer diagnosis and treatment initiation.
Unveiling The Factors That Delay Cancer Detection:
• Lack of Awareness and Education:
Limited awareness among patients and healthcare providers about the signs and symptoms of cancer can contribute to delays in seeking medical attention and timely referral for diagnostic evaluation.
• Symptom Misinterpretation:
Patients may misinterpret cancer symptoms as benign or attribute them to other less serious conditions, leading to delays in seeking medical care and diagnostic assessment.
• Healthcare Access Barriers:
Socioeconomic factors, including financial constraints, lack of health insurance, transportation issues, and geographical barriers, can hinder access to primary care services and diagnostic tests, delaying cancer detection.
• Provider Factors:
Healthcare providers may overlook or misinterpret cancer symptoms, leading to delays in referral for further evaluation or diagnostic testing. Inadequate training, time constraints, and competing clinical priorities may contribute to diagnostic delays.
• Diagnostic Delays:
Challenges in obtaining timely diagnostic tests, such as imaging studies, biopsies, or laboratory tests, can prolong the time to cancer diagnosis. Delays in test scheduling, availability of specialized services, and interpretation of test results may further exacerbate diagnostic delays.
• Patient Factors:
Patient-related factors, including fear, denial, stigma associated with cancer, language barriers, and cultural beliefs, can influence help-seeking behavior and delay presentation to healthcare providers for evaluation of symptoms.
• Delayed Referrals and Consultations:
Delays in referral from primary care providers to specialists, such as oncologists or surgeons, and in scheduling appointments for consultations or diagnostic procedures can contribute to prolonged time to cancer diagnosis.
• Communication Challenges:
Poor communication between healthcare providers, inadequate sharing of medical information, and fragmented care coordination can lead to delays in diagnostic evaluation and treatment initiation.
• Diagnostic Errors:
Diagnostic errors, including misdiagnosis or delayed diagnosis of cancer, can occur due to a variety of factors, such as atypical presentation of symptoms, interpretation errors, or inadequate follow-up of abnormal findings.
• Systemic Issues:
Structural deficiencies in healthcare systems, such as limited resources, overcrowded clinics, long wait times for appointments or diagnostic tests, and insufficient capacity to meet patient demand, can contribute to delays in cancer detection and treatment.
Adjunctive Methods For Early Detection
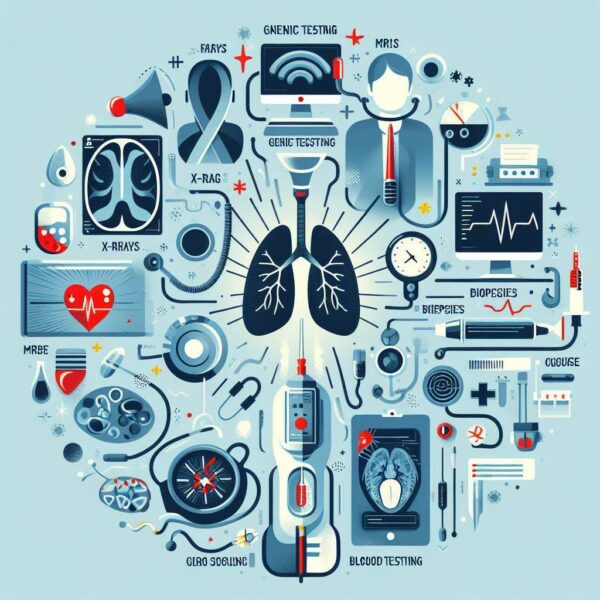
Early detection plays a pivotal role in improving outcomes for various medical conditions, including cancer. While traditional screening methods are valuable, adjunctive methods offer additional tools for enhancing early detection efforts.
These supplementary approaches complement existing screening modalities, providing healthcare providers with a more comprehensive toolkit for identifying diseases in their earliest stages. In this article, we delve into the realm of adjunctive methods for early detection, exploring their benefits, applications, and potential impact on patient care.
By shedding light on these innovative approaches, we aim to underscore the importance of a multifaceted approach to early disease detection and highlight the potential of adjunctive methods in improving health outcomes.
Exploring Adjunctive Methods:
1. Biological Markers:
Biomarkers, such as proteins, DNA, RNA, and metabolites, can serve as indicators of disease presence or progression. Biomarker assays enable non-invasive detection of specific molecules associated with disease, offering a potential avenue for early diagnosis and monitoring of treatment response.
2. Imaging Techniques:
Advanced imaging modalities, including MRI, PET-CT, and molecular imaging, provide detailed anatomical and functional information about tissues and organs. These techniques allow for the visualization of abnormalities that may not be detectable with conventional screening methods, facilitating early detection of cancer and other diseases.
3. Liquid Biopsies:
Liquid biopsy techniques involve the analysis of biomarkers, such as circulating tumor cells (CTCs), cell-free DNA (cfDNA), and exosomes, in bodily fluids such as blood, urine, or saliva. These minimally invasive tests offer a non-invasive means of detecting cancer and monitoring disease progression in real-time.
4. Genomic Testing:
Genomic testing examines the genetic makeup of an individual’s cells to identify mutations or alterations associated with disease risk or progression. Next-generation sequencing (NGS) technologies enable comprehensive genomic profiling, allowing for personalized risk assessment and early detection of genetic conditions and cancers.
5. Artificial Intelligence (AI):
AI-powered algorithms analyze large datasets, including medical imaging studies and electronic health records, to identify patterns and anomalies indicative of disease. AI-driven diagnostic tools can assist healthcare providers in interpreting complex data and identifying subtle signs of disease at an early stage.
6. Microbiome Analysis:
The human microbiome, comprising trillions of microorganisms inhabiting the body, plays a crucial role in health and disease. Microbiome analysis techniques enable the identification of microbial signatures associated with various conditions, offering insights into disease pathogenesis and early detection strategies.
7. Point-of-Care Testing:
Point-of-care (POC) testing devices provide rapid and convenient diagnostic results at the bedside or in clinical settings. These portable devices enable early detection of infectious diseases, metabolic disorders, and other conditions, facilitating timely intervention and management.
8. Telemedicine and Remote Monitoring:
Telemedicine platforms and remote monitoring technologies allow for the remote assessment and monitoring of patient’s health status. Virtual consultations, wearable devices, and smartphone applications enable early detection of disease symptoms and facilitate timely intervention, particularly in underserved or remote communities.
9. Mass Spectrometry:
Mass spectrometry techniques analyze molecular signatures in biological samples, such as tissues or bodily fluids, to detect disease-specific markers. Mass spectrometry-based assays offer high sensitivity and specificity for early disease detection, making them valuable tools in clinical diagnostics.
10. Nanotechnology:
Nanotechnology-based sensors and devices leverage nanoscale materials and structures to detect disease biomarkers with high sensitivity and specificity. These miniature devices enable early detection of cancer, infectious diseases, and other conditions, paving the way for personalized medicine and targeted therapies.
Improving Screening Abilities And Advising On Primary Prevention

Screening for diseases plays a critical role in preventive healthcare, enabling early detection and intervention to improve patient outcomes. However, the effectiveness of screening programs relies not only on the availability of screening tests but also on the integration of primary prevention strategies.
By enhancing screening abilities and offering comprehensive guidance on primary prevention measures, healthcare systems can optimize their efforts to combat diseases and promote overall well-being.
In this article, we explore strategies for improving screening abilities and advising on primary prevention, aiming to empower individuals to take proactive steps toward maintaining their health and preventing the onset of diseases.
Expanding Screening Programs:
Increasing access to screening tests and services, particularly for high-risk populations, can enhance early detection of diseases such as cancer, cardiovascular conditions, and infectious diseases.
• Utilizing Advanced Screening Technologies:
Embracing technological advancements, such as genomic testing, biomarker assays, and imaging modalities, can improve the accuracy and reliability of screening tests, enabling earlier detection of diseases.
• Implementing Population-Based Screening Initiatives:
Developing population-based screening programs tailored to the specific needs and risk profiles of different communities can increase screening uptake and reduce disparities in healthcare access and outcomes.
• Promoting Screening Awareness and Education:
Educating the public about the importance of screening for various diseases and raising awareness about available screening programs can encourage individuals to participate in screening and seek timely healthcare services.
• Integrating Primary Prevention Measures:
Incorporating primary prevention strategies, such as lifestyle modifications, vaccination programs, and environmental interventions, into healthcare practices can address underlying risk factors and reduce the incidence of diseases.
• Encouraging Healthy Lifestyle Behaviors:
Advising individuals to adopt healthy behaviors, including regular exercise, balanced nutrition, smoking cessation, and moderation in alcohol consumption, can mitigate disease risk factors and promote overall well-being.
• Facilitating Access to Preventive Services:
Ensuring equitable access to preventive healthcare services, such as vaccinations, counseling, and health screenings, can empower individuals to take proactive steps towards disease prevention and early detection.
• Promoting Community Engagement and Collaboration:
Engaging communities, healthcare providers, policymakers, and other stakeholders in collaborative efforts to promote screening and primary prevention can foster a supportive environment for preventive healthcare initiatives.
• Tailoring Prevention Strategies to Individual Needs:
Recognizing that one size does not fit all, healthcare providers should tailor prevention recommendations to individual risk factors, preferences, and socio-cultural backgrounds to maximize effectiveness and adherence.
• Monitoring and Evaluating Screening Programs:
Implementing robust monitoring and evaluation mechanisms to assess the effectiveness, accessibility, and impact of screening programs and primary prevention interventions can inform future strategies and enhance outcomes.
Why It’s Done
In the realm of healthcare, various medical procedures and interventions are performed to diagnose, treat, or prevent diseases, injuries, or other health conditions. Understanding the rationale behind why these procedures are done is crucial for patients and healthcare providers alike.
From diagnostic tests to surgical interventions, each procedure serves a specific purpose aimed at improving patient outcomes and enhancing quality of life. In this article, we delve into the significance of why medical procedures are performed, exploring the underlying reasons and objectives behind common healthcare practices.
By gaining insights into the purpose behind these procedures, individuals can make informed decisions about their healthcare, and healthcare providers can deliver more effective and patient-centered care.
Understanding the Purpose Behind Medical Procedures:
1. Diagnostic Purposes:
Medical procedures are often performed to diagnose underlying health conditions or to confirm suspected diagnoses. Diagnostic tests such as imaging studies, blood tests, and biopsies help healthcare providers identify the cause of symptoms and formulate appropriate treatment plans.
2. Treatment and Intervention:
Medical procedures may be carried out to treat existing health conditions, alleviate symptoms, or prevent disease progression. These interventions can include medications, surgeries, therapies, or minimally invasive procedures aimed at addressing specific health issues.
3. Preventive Healthcare:
Certain medical procedures are performed as part of preventive healthcare efforts to detect and mitigate potential health risks before they develop into serious conditions. Examples include vaccinations, cancer screenings, and routine health check-ups.
4. Monitoring and Management:
Medical procedures may be conducted to monitor disease progression, assess treatment effectiveness, or manage chronic conditions. Regular monitoring through tests, imaging studies, or clinical assessments helps healthcare providers track patient health and adjust treatment plans as needed.
5. Diagnostic Confirmation:
In some cases, medical procedures are performed to confirm or rule out a diagnosis based on initial findings or clinical suspicions. These confirmatory tests provide definitive information to guide treatment decisions and ensure accurate diagnosis.
6. Risk Assessment and Prognosis:
Certain medical procedures, such as genetic testing, biomarker analysis, or prognostic assessments, are conducted to evaluate individual risk factors, predict disease outcomes, or tailor treatment approaches based on personalized patient characteristics.
7. Research and Advancements:
Medical procedures may be performed as part of clinical trials, research studies, or technological advancements aimed at improving healthcare outcomes, developing new treatments, or enhancing diagnostic capabilities.
8. Patient Education and Empowerment:
Some medical procedures serve an educational purpose, providing patients with valuable information about their health status, treatment options, and self-management strategies. Empowered patients are better equipped to participate in their healthcare decisions and engage in preventive behaviors.
9. Emergency Situations:
In emergency situations, medical procedures are performed to stabilize patients, address life-threatening conditions, or prevent further harm. These interventions prioritize patient safety and survival, often requiring swift and decisive action.
10. Quality of Life Improvement:
Medical procedures may be undertaken to improve patients’ quality of life, alleviate symptoms, or restore functional abilities. These interventions aim to enhance overall well-being and promote patient comfort and independence.
Why Are Oral Cancer Screenings So Important?

Oral cancer is a serious and potentially life-threatening disease that affects millions of people worldwide. Early detection plays a crucial role in improving treatment outcomes and increasing survival rates for individuals diagnosed with oral cancer.
Oral cancer screenings are essential preventive measures that help identify abnormalities in the mouth and throat before they progress into cancerous lesions. In this article, we explore the importance of oral cancer screenings and why they are vital for maintaining optimal oral health.
By understanding the significance of regular screenings, individuals can take proactive steps to protect themselves against the risks associated with oral cancer and ensure early detection and timely intervention if needed.
The Significance of Oral Cancer Screenings:
• Early Detection Saves Lives:
Oral cancer screenings facilitate the early detection of abnormal tissue changes, allowing for prompt diagnosis and treatment initiation. Early-stage oral cancer is highly treatable, with significantly better outcomes compared to advanced-stage disease.
• Risk Identification and Prevention:
Screening helps identify individuals at higher risk for oral cancer due to factors such as tobacco use, alcohol consumption, HPV infection, and family history. By identifying risk factors early, healthcare providers can implement preventive measures and lifestyle interventions to reduce the likelihood of cancer development.
• Non-Invasive and Painless:
Oral cancer screenings are typically quick, non-invasive, and painless procedures that can be performed during routine dental check-ups or medical examinations. The process involves visual inspection of the oral cavity and palpation of the head and neck for suspicious lesions or abnormalities.
• Detecting Precancerous Lesions:
In addition to detecting early-stage cancers, screenings can identify precancerous lesions or oral dysplasia, which have the potential to progress into invasive cancer if left untreated. Early intervention for precancerous lesions can prevent the development of oral cancer.
• Improving Treatment Outcomes:
Early detection of oral cancer allows for less invasive treatment options, such as surgical excision or targeted therapies, which are associated with fewer side effects and better preservation of oral function and aesthetics.
• Reducing Healthcare Costs:
Timely detection and treatment of oral cancer through screenings can result in cost savings for both patients and healthcare systems by avoiding the need for more extensive and expensive treatments for advanced-stage disease.
• Educating Patients and Promoting Awareness:
Oral cancer screenings provide opportunities for patient education and awareness about the signs, symptoms, and risk factors associated with oral cancer. By raising awareness and promoting regular screenings, healthcare providers can empower individuals to prioritize their oral health and seek timely medical attention if needed.
• Monitoring High-Risk Populations:
Individuals with known risk factors for oral cancer, such as tobacco users, heavy drinkers, and those with a family history of the disease, benefit from regular screenings to monitor their oral health status and detect any changes early.
• Comprehensive Oral Health Care:
Incorporating oral cancer screenings into routine dental and medical care promotes a holistic approach to oral health and wellness, emphasizing the importance of early detection and prevention in maintaining overall well-being.
• Supporting Public Health Initiatives:
Oral cancer screenings contribute to public health initiatives aimed at reducing the burden of oral cancer on society by identifying cases early, facilitating timely treatment, and ultimately improving survival rates and quality of life for affected individuals.
Can A Dentist See If You Have Oral Cancer?

Oral cancer is a serious and potentially life-threatening condition that affects thousands of individuals each year. Early detection is crucial for successful treatment and improved outcomes. Many people wonder whether their dentist can detect oral cancer during a routine dental examination.
In this article, we explore the role of dentists in identifying oral cancer, the signs and symptoms they may observe, and the importance of regular dental check-ups in oral cancer screening.
Understanding the capabilities of dentists in detecting oral cancer can empower individuals to prioritize their oral health and seek timely medical attention if needed.
• Visual Examination:
Dentists are trained to perform thorough visual examinations of the oral cavity, including the lips, gums, tongue, cheeks, and throat. During a dental check-up, dentists look for any abnormal changes or lesions that may indicate oral cancer.
• Palpation of Tissues:
In addition to visual inspection, dentists may palpate or feel the tissues of the mouth and neck to detect any lumps, bumps, or areas of induration (hardening) that could be suggestive of underlying pathology, including oral cancer.
• Evaluation of Risk Factors:
Dentists assess a patient’s medical history and lifestyle factors, such as tobacco use, alcohol consumption, HPV infection, sun exposure, and family history of cancer, to determine their risk of developing oral cancer.
• Identification of Suspicious Lesions:
Dentists are trained to recognize various types of oral lesions, including leukoplakia (white patches), erythroplakia (red patches), and ulcerations, which may raise suspicion for oral cancer. Any suspicious lesions may prompt further investigation or referral for biopsy.
• Use of Adjunctive Tools:
Some dental practices utilize adjunctive screening tools, such as oral cancer screening devices or fluorescence visualization devices, to aid in the early detection of oral cancer. These tools can help dentists identify abnormalities that may not be visible to the naked eye.
• Patient Education and Awareness:
Dentists play a crucial role in educating patients about the signs and symptoms of oral cancer, as well as the importance of regular dental check-ups and screenings for early detection. By raising awareness and promoting preventive measures, dentists empower patients to take proactive steps towards oral health.
• Referral for Further Evaluation:
If a dentist suspects oral cancer based on clinical findings or risk factors, they may refer the patient to a specialist, such as an oral and maxillofacial surgeon or an oral pathologist, for further evaluation, biopsy, and definitive diagnosis.
• Regular Monitoring and Follow-Up:
For patients at increased risk of oral cancer, dentists may recommend regular monitoring and follow-up appointments to monitor for any changes or new developments in oral health status and to facilitate early detection of recurrence or new lesions.
• Promotion of Healthy Habits:
Dentists emphasize the importance of maintaining good oral hygiene practices, quitting smoking, limiting alcohol consumption, practicing sun safety, and receiving HPV vaccination as part of oral cancer prevention efforts.
Conclusion:
Screening for oral cancer is a vital component of preventive healthcare, allowing for the early detection and intervention of this potentially life-threatening condition. By undergoing regular oral cancer screenings, individuals can significantly increase their chances of successful treatment and improved outcomes.
Dentists play a crucial role in the screening process, utilizing their expertise to conduct thorough examinations, identify suspicious lesions, and educate patients about the importance of early detection.
Through collaboration with other healthcare providers and the promotion of healthy lifestyle habits, dentists contribute to the overall well-being of their patients and help reduce the burden of oral cancer on society.
FAQs:
Q1: What are the risk factors for developing oral cancer?
A: Risk factors for oral cancer include tobacco use, excessive alcohol consumption, HPV infection, sun exposure, poor oral hygiene, and a family history of cancer.
Q2: Can oral cancer affect individuals of any age?
A: While oral cancer is more common in older adults, it can affect individuals of any age, including young adults and adolescents.
Q3: Are there any warning signs or symptoms of oral cancer to watch out for?
A: Warning signs of oral cancer may include persistent mouth sores, unexplained bleeding, lumps or thickening in the mouth or throat, difficulty swallowing or chewing, and changes in voice or speech.
Q4: How often should I undergo oral cancer screenings?
A: The frequency of oral cancer screenings may vary depending on individual risk factors and dental history. It is generally recommended to undergo screenings at least once a year during routine dental check-ups.
Q5: Can oral cancer be prevented?
A: While not all cases of oral cancer can be prevented, individuals can reduce their risk by avoiding tobacco and alcohol use, practicing good oral hygiene, limiting sun exposure, receiving HPV vaccination, and attending regular dental check-ups for screenings and early detection.
