In recent years, the landscape of diabetes management has seen significant advancements, one of which is the introduction of Ozempic. This medication has garnered attention for its efficacy in managing type 2 diabetes, providing patients with an additional treatment option to help control blood sugar levels.
Understanding Ozempic and its usage is essential for individuals living with diabetes and healthcare professionals alike. In this article, we’ll delve into the intricacies of Ozempic, exploring how it works, its benefits, potential side effects, and guidelines for usage.
By gaining insight into this medication, individuals can make informed decisions about their diabetes treatment plan, working closely with their healthcare providers to achieve optimal health outcomes.
Understanding Ozempic And Its Usage
Ozempic, also known by its generic name semaglutide, belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists. It works by mimicking the action of incretin hormones in the body, which help regulate blood sugar levels by stimulating insulin release, slowing down gastric emptying, and reducing appetite.
Here’s a comprehensive look at Ozempic and its usage:
Mechanism of Action:
Ozempic works by activating GLP-1 receptors in the pancreas, leading to increased insulin secretion in response to elevated blood sugar levels. It also inhibits glucagon secretion, which helps prevent excess glucose production by the liver.
Additionally, Ozempic slows down the rate at which food moves through the stomach, leading to a feeling of fullness and reduced appetite.
Benefits:
Ozempic offers several benefits for individuals with type 2 diabetes, including improved glycemic control, reduced risk of hypoglycemia (low blood sugar), and potential weight loss.
Clinical trials have shown that Ozempic can help lower HbA1c levels and may also have cardiovascular benefits, such as reducing the risk of heart attack and stroke.
Dosage and Administration:
Ozempic is typically administered once weekly via subcutaneous injection. The starting dose is usually 0.25 mg once weekly, with the option to increase to 0.5 mg or 1 mg based on individual response and tolerability.
It is important to follow the dosing instructions provided by your healthcare provider and to administer the medication as directed.
Considerations and Precautions:
Before starting Ozempic, it is important to discuss any pre-existing medical conditions, allergies, or medications you may be taking with your healthcare provider. Ozempic may not be suitable for everyone, especially individuals with a history of pancreatitis or thyroid disease. Pregnant or breastfeeding women should also consult with their healthcare provider before using Ozempic. I hope now you Understanding Ozempic And Its Usage.
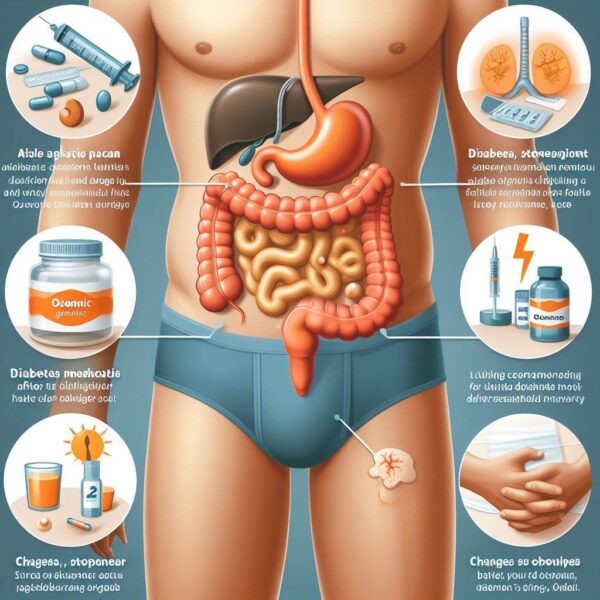
Side Effects Of Ozempic
Managing type 2 diabetes often involves a combination of lifestyle changes, medications, and regular monitoring of blood sugar levels. Ozempic, a medication belonging to the class of glucagon-like peptide-1 (GLP-1) receptor agonists, has emerged as a valuable treatment option for individuals with type 2 diabetes.
However, like any medication, Ozempic may be associated with certain side effects that individuals should be aware of. Understanding the potential side effects of Ozempic is essential for patients and healthcare providers to make informed decisions about its usage.
Understanding the common and rare side effects of Ozempic, how they may manifest, and when to seek medical attention if they occur. By understanding these side effects, individuals can better manage their diabetes treatment and minimize any potential risks associated with Ozempic usage.
Side Effects:
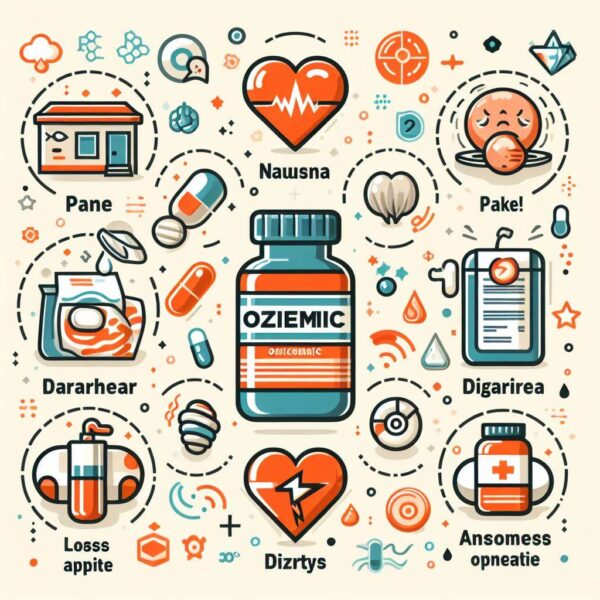
While Ozempic is generally well-tolerated, it may cause side effects in some individuals. Here are the common and rare side effects of Ozempic:
Nausea:
Nausea is one of the most common side effects reported by individuals taking Ozempic. It may occur during the initial weeks of treatment but often improves over time as the body adjusts to the medication. Eating smaller, more frequent meals and avoiding spicy or greasy foods may help alleviate nausea.
Vomiting:
Some individuals may experience vomiting as a side effect of Ozempic. Like nausea, vomiting may occur early in the treatment but tends to diminish with continued use of the medication. Staying hydrated and avoiding heavy meals may help reduce the likelihood of vomiting.
Diarrhea:
Diarrhea is another gastrointestinal side effect that may occur with Ozempic use. It is characterized by loose or watery stools and may be accompanied by abdominal cramping. Drinking plenty of fluids and consuming high-fiber foods can help manage diarrhea.
Abdominal Pain:
Abdominal pain or discomfort may occur in some individuals taking Ozempic. This may be due to gastrointestinal disturbances caused by the medication. If abdominal pain persists or becomes severe, it is important to consult a healthcare provider for evaluation.
Constipation:
In contrast to diarrhea, some individuals may experience constipation while taking Ozempic. Constipation is characterized by infrequent bowel movements and difficulty passing stool. Increasing fiber intake, staying hydrated, and engaging in regular physical activity can help alleviate constipation.
Pancreatitis:
In rare cases, Ozempic may increase the risk of pancreatitis, and inflammation of the pancreas. Symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, and fever. If you experience these symptoms while taking Ozempic, seek medical attention immediately, as pancreatitis can be a serious condition.
Hypoglycemia:
Ozempic may lower blood sugar levels, leading to hypoglycemia (low blood sugar) in some individuals, especially when used in combination with other diabetes medications such as insulin or sulfonylureas. Symptoms of hypoglycemia include sweating, trembling, confusion, and fainting. It is important to monitor blood sugar levels regularly and be prepared to treat hypoglycemia if it occurs.
Allergic Reactions:
While rare, some individuals may experience allergic reactions to Ozempic, characterized by symptoms such as rash, itching, swelling of the face or throat, and difficulty breathing. If you experience any signs of an allergic reaction, seek immediate medical attention.
It is essential to discuss any side effects or concerns with your healthcare provider while taking Ozempic. Your healthcare provider can offer guidance on managing side effects and may adjust your treatment plan if necessary.
With proper monitoring and management, many individuals can benefit from the therapeutic effects of Ozempic while minimizing the risk of side effects.
What Is The Role Of The Gallbladder In Our Body?
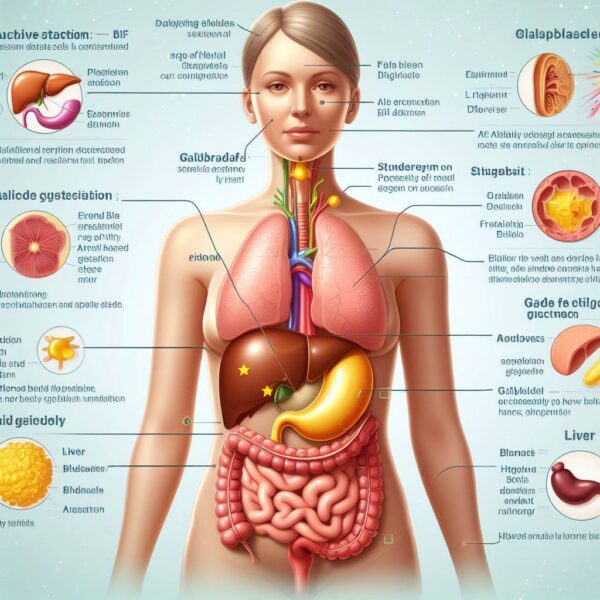
The gallbladder is a small, pear-shaped organ located beneath the liver, and while it often goes unnoticed, its role in the digestive process is crucial. This remarkable organ plays a significant role in storing and concentrating bile, a digestive fluid produced by the liver.
Bile aids in the digestion and absorption of fats in the small intestine, facilitating the breakdown of dietary fats into smaller molecules that can be absorbed by the body. Understanding the role of the gallbladder in our body is essential for comprehending how the digestive system functions and how disruptions to its normal function can impact our health.
Knowing the intricate role of the gallbladder in digestion, its importance in maintaining digestive health, and how certain conditions affecting the gallbladder can lead to digestive problems and other complications.
The Role Of The Gallbladder:
The gallbladder plays a vital role in the digestive process, primarily by storing and concentrating bile produced by the liver. Bile is a yellowish-green fluid composed of water, bile salts, cholesterol, bilirubin, and other compounds. It is produced by the liver and then stored and concentrated in the gallbladder until it is needed for digestion.
Here’s a detailed look at the role of the gallbladder in our body:
Storage and Concentration of Bile:
The primary function of the gallbladder is to store and concentrate bile between meals. When we eat, the gallbladder contracts and releases bile into the small intestine to aid in the digestion and absorption of fats.
Emulsification of Fats:
Bile contains bile salts, which help emulsify fats in the small intestine. Emulsification breaks down large fat globules into smaller droplets, increasing the surface area for enzymes to act upon and facilitating the digestion of fats.
Facilitation of Fat Digestion:
Bile plays a crucial role in the digestion of dietary fats. It helps solubilize fats and fat-soluble vitamins, such as vitamins A, D, E, and K, allowing them to be absorbed through the intestinal lining into the bloodstream.
Neutralization of Stomach Acid:
Bile also helps neutralize stomach acid that enters the small intestine, creating a more favorable environment for the activity of pancreatic enzymes involved in digestion.
Elimination of Waste Products:
In addition to aiding in digestion, bile helps eliminate waste products, such as bilirubin, from the body. Bilirubin is a yellow pigment produced from the breakdown of red blood cells and is excreted in bile.
Regulation of Cholesterol Metabolism:
The gallbladder also plays a role in cholesterol metabolism by concentrating bile and recycling cholesterol from bile back to the liver for reprocessing.
Overall, the gallbladder plays a crucial role in the digestive process by storing, concentrating, and releasing bile to aid in the digestion and absorption of fats.
Dysfunction of the gallbladder or disruptions to bile flow can lead to digestive problems, such as gallstones, biliary colic, and other complications, highlighting the importance of maintaining gallbladder health for overall digestive well-being.
How To Manage A Diabetic Condition After Gallbladder Removal
Living with diabetes requires careful management to maintain optimal health and well-being. However, managing diabetes can become more challenging for individuals who have undergone gallbladder removal surgery, also known as cholecystectomy.
The gallbladder plays a crucial role in the digestive process by storing and releasing bile to aid in the digestion of fats. Without a gallbladder, the digestive system may be altered, potentially impacting blood sugar levels and diabetes management. In this article, we will explore strategies for managing a diabetic condition after gallbladder removal surgery.
By understanding how the absence of the gallbladder can affect digestion and blood sugar control, individuals can implement lifestyle modifications and dietary adjustments to effectively manage their diabetes and maintain overall health.
Managing A Diabetic Condition:
Gallbladder removal surgery, whether performed laparoscopically or through open surgery, can have implications for digestion and nutrient absorption, which may affect blood sugar control in individuals with diabetes. Here are some strategies for managing a diabetic condition after gallbladder removal:
1. Monitor Blood Sugar Levels Regularly:
After gallbladder removal, it is essential to monitor blood sugar levels regularly to assess how dietary changes and other factors may affect blood glucose levels. Frequent monitoring can help identify patterns and trends, allowing for adjustments to diabetes management strategies as needed.
2. Adopt a Low-Fat Diet:
Following gallbladder removal, some individuals may experience difficulty digesting fats, leading to symptoms such as bloating, gas, and diarrhea. To minimize digestive discomfort and maintain stable blood sugar levels, consider adopting a low-fat diet that focuses on lean proteins, whole grains, fruits, and vegetables.
3. Eat Smaller, More Frequent Meals:
Consuming smaller, more frequent meals throughout the day can help alleviate digestive symptoms and prevent fluctuations in blood sugar levels. Aim to eat every few hours and avoid large, heavy meals that may overwhelm the digestive system.
4. Choose Healthy Fats Wisely:
While it’s important to limit dietary fat intake after gallbladder removal, incorporating healthy fats into your diet can provide essential nutrients and support overall health. Opt for sources of healthy fats such as avocados, nuts, seeds, and fatty fish, and avoid fried and greasy foods.
5. Stay Hydrated:
Adequate hydration is essential for proper digestion and overall health, especially after gallbladder removal. Drink plenty of water throughout the day to help flush out toxins, support digestion, and prevent dehydration, which can affect blood sugar levels.
6. Consider Digestive Enzyme Supplements:
In some cases, individuals may benefit from taking digestive enzyme supplements to help aid in the digestion of fats and alleviate digestive discomfort after gallbladder removal. Consult with a healthcare provider or registered dietitian to determine if enzyme supplements are appropriate for you.
7. Manage Stress Levels:
Stress can impact blood sugar levels and digestive function, so it’s important to incorporate stress-reducing activities into your daily routine. Practice relaxation techniques such as deep breathing, meditation, yoga, or tai chi to help manage stress and promote overall well-being.
8. Work with Healthcare Providers:
Lastly, work closely with your healthcare providers, including your primary care physician, endocrinologist, and registered dietitian, to develop a personalized diabetes management plan tailored to your individual needs and medical history.
They can provide guidance, support, and ongoing monitoring to help you effectively manage your diabetic condition after gallbladder removal.
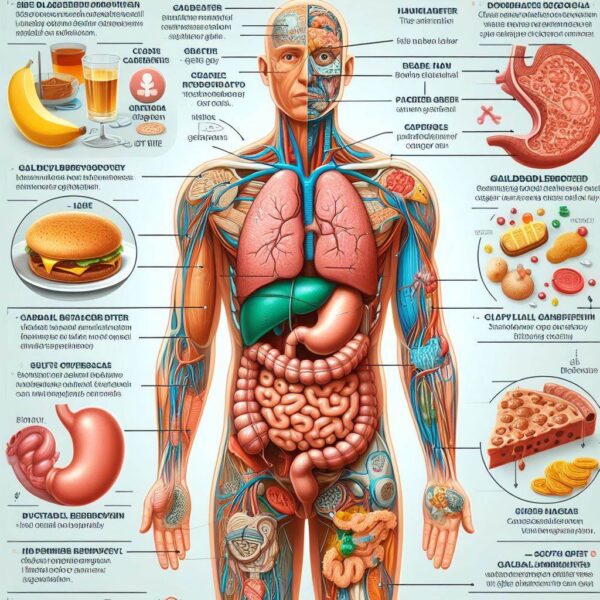
Impact Of Gallbladder Removal On Diabetes Management
The management of diabetes is a complex undertaking that involves various lifestyle modifications, medications, and monitoring to keep blood sugar levels within a healthy range. However, for individuals who have undergone gallbladder removal surgery, also known as cholecystectomy, managing diabetes may present additional challenges.
The gallbladder plays a crucial role in the digestive process by storing and releasing bile, which aids in the digestion of fats. Without a gallbladder, the digestive system may be altered, potentially impacting nutrient absorption and blood sugar control. In this article, we will explore the impact of gallbladder removal on diabetes management.
By understanding how the absence of the gallbladder can affect digestion, nutrient absorption, and blood sugar levels, individuals with diabetes can work with healthcare providers to develop strategies for optimal diabetes management post-cholecystectomy.
Impact Of Gallbladder Removal:
Gallbladder removal surgery can have several implications for diabetes management due to its effects on digestion, nutrient absorption, and bile flow. Here are some ways in which gallbladder removal may impact diabetes management:
Altered Fat Digestion:
The gallbladder plays a crucial role in the digestion of fats by storing and releasing bile, which helps emulsify fats in the small intestine. Without a gallbladder, bile may continuously drip into the small intestine rather than being released in response to food intake.
This can lead to difficulty digesting fats, resulting in symptoms such as bloating, gas, and diarrhea.
Changes in Nutrient Absorption:
In addition to fat digestion, the gallbladder also plays a role in the absorption of fat-soluble vitamins, such as vitamins A, D, E, and K. Without adequate bile flow, individuals may experience reduced absorption of these vitamins, which are essential for overall health and may impact blood sugar control.
Potential for Nutritional Deficiencies:
Reduced fat digestion and impaired absorption of fat-soluble vitamins after gallbladder removal may increase the risk of nutritional deficiencies in individuals with diabetes. Deficiencies in vitamins and minerals can affect overall health and may exacerbate diabetes-related complications.
Impact on Blood Sugar Levels:
Changes in digestion and nutrient absorption after gallbladder removal can affect blood sugar levels in individuals with diabetes. Fluctuations in blood sugar levels may occur due to alterations in food digestion and nutrient absorption, requiring adjustments to diabetes management strategies.
Gastrointestinal Symptoms:
Some individuals may experience gastrointestinal symptoms such as abdominal pain, bloating, gas, and diarrhea after gallbladder removal, which can impact dietary choices and blood sugar control. Managing these symptoms effectively is essential for maintaining overall well-being and diabetes management.
Individual Variation:
It’s important to note that the impact of gallbladder removal on diabetes management can vary from person to person. While some individuals may experience significant digestive issues and changes in blood sugar control, others may have minimal or no symptoms.
Factors such as diet, lifestyle, pre-existing digestive conditions, and the extent of gallbladder dysfunction prior to surgery can influence the outcomes post-cholecystectomy.
Personalized Approach to Management:
Given the variability in how gallbladder removal may affect diabetes management, it’s essential for individuals to work closely with their healthcare providers to develop a personalized approach to diabetes management post-cholecystectomy.
This may involve dietary modifications, medication adjustments, regular monitoring of blood sugar levels, and addressing any gastrointestinal symptoms or nutritional deficiencies that arise.
Importance Of Ozempic In Managing Diabetes After Surgery

Managing diabetes after surgery presents unique challenges, as surgical procedures can impact blood sugar levels and require adjustments to diabetes management strategies. Ozempic, a medication belonging to the class of glucagon-like peptide-1 (GLP-1) receptor agonists, has emerged as a valuable treatment option for individuals with type 2 diabetes.
Its role in managing diabetes after surgery is particularly significant due to its ability to improve blood sugar control, promote weight loss, and reduce the risk of cardiovascular events.
By understanding how Ozempic works and its benefits in the post-surgical setting, individuals and healthcare providers can make informed decisions about its use to optimize diabetes management outcomes.
Importance Of Ozempic:
Managing diabetes after surgery requires a multifaceted approach to address the physiological changes that occur during the recovery period. Ozempic plays a crucial role in diabetes management after surgery due to its various benefits, including:
Improved Blood Sugar Control:
Ozempic works by mimicking the effects of a hormone called glucagon-like peptide-1 (GLP-1), which stimulates insulin secretion and inhibits glucagon release, leading to improved blood sugar control.
After surgery, blood sugar levels may fluctuate due to changes in diet, medication absorption, and stress responses. Ozempic helps stabilize blood sugar levels, reducing the risk of hyperglycemia and hypoglycemia post-surgery.
Weight Loss Promotion:
Weight management is essential for individuals with diabetes, especially after surgery, as excess weight can exacerbate diabetes-related complications. Ozempic has been shown to promote weight loss by reducing appetite, increasing feelings of fullness, and slowing gastric emptying.
This can help individuals achieve and maintain a healthy weight, improving overall diabetes management outcomes.
Cardiovascular Risk Reduction:
Individuals with diabetes are at increased risk of cardiovascular events such as heart attack and stroke. Ozempic has demonstrated cardiovascular benefits, including reducing the risk of major adverse cardiovascular events (MACE) in clinical trials.
By lowering blood sugar levels and promoting weight loss, Ozempic helps mitigate cardiovascular risk factors in individuals with diabetes after surgery.
Flexible Administration:
Ozempic is available in a convenient once-weekly injectable formulation, providing flexibility and ease of administration for individuals managing diabetes after surgery. This dosing schedule simplifies medication adherence and reduces the burden of daily injections, allowing individuals to focus on their recovery and overall well-being.
Potential for Post-Surgical Complication Prevention:
Adequate blood sugar control is essential for preventing post-surgical complications such as infections, delayed wound healing, and cardiovascular events. By optimizing blood sugar levels, Ozempic may help reduce the risk of these complications and support a smoother recovery process after surgery.
Long-Lasting Effects:
Ozempic has a long duration of action, providing sustained blood sugar control throughout the week with once-weekly dosing. This consistency in medication delivery helps maintain stable blood sugar levels, reducing the risk of glycemic fluctuations and associated complications after surgery.
Side Effects Of Gallbladder Removal On The Body
Gallbladder removal surgery, also known as cholecystectomy, is a common procedure performed to address gallbladder-related conditions such as gallstones, inflammation, or infection.
While the removal of the gallbladder can alleviate symptoms and improve quality of life for many individuals, it can also have various effects on the body.
Understanding the potential side effects of gallbladder removal is essential for individuals considering or undergoing this procedure. By gaining insight into these potential effects, individuals can make informed decisions about their healthcare and prepare for any changes they may experience post-surgery.
Side Effects:
Gallbladder removal surgery is typically considered safe and effective, but like any surgical procedure, it can have potential side effects and complications. Here are some common side effects of gallbladder removal on the body:
1. Digestive Symptoms:
One of the most common side effects of gallbladder removal is digestive symptoms such as diarrhea, bloating, gas, and indigestion. Without a gallbladder to store and concentrate bile, bile may continuously drip into the small intestine, leading to difficulty digesting fats and disrupting the normal digestive process.
2. Increased Risk of Bile Reflux:
Without the gallbladder to regulate bile flow, some individuals may experience bile reflux, where bile flows backward into the stomach or esophagus. Bile reflux can cause symptoms such as heartburn, nausea, and a bitter taste in the mouth, similar to acid reflux.
3. Difficulty Digesting Fatty Foods:
The gallbladder stores and releases bile in response to the ingestion of fatty foods, aiding in their digestion. After gallbladder removal, some individuals may have difficulty digesting fatty foods, leading to symptoms such as abdominal pain, cramping, and diarrhea, particularly after meals high in fat content.
4. Changes in Bowel Habits:
Gallbladder removal can disrupt normal bowel habits, leading to changes such as increased frequency of bowel movements or loose stools. Some individuals may experience diarrhea shortly after eating, especially meals high in fat, due to the lack of bile storage and regulation.
5. Nutritional Deficiencies:
The gallbladder plays a role in the absorption of fat-soluble vitamins such as vitamins A, D, E, and K. Without adequate bile flow, individuals may be at risk of nutritional deficiencies in these vitamins, which are essential for various bodily functions and overall health.
6. Long-Term Risk of Gallstone Formation:
In some cases, individuals who undergo gallbladder removal may develop gallstones in the bile ducts or remnants of the gallbladder, known as residual or retained stones. These stones can cause symptoms similar to those of gallstones, such as abdominal pain, jaundice, and pancreatitis.
7. Potential for Sphincter of Oddi Dysfunction:
Sphincter of Oddi dysfunction is a condition characterized by dysfunction of the sphincter muscle that controls the flow of bile and pancreatic juices into the small intestine. Gallbladder removal can increase the risk of sphincter Oddi dysfunction, leading to symptoms such as abdominal pain, nausea, and vomiting.
8. Risk of Postcholecystectomy Syndrome:
Postcholecystectomy syndrome refers to a collection of symptoms that persist or develop after gallbladder removal, including abdominal pain, bloating, gas, and diarrhea. This syndrome can occur due to various factors, such as bile duct stones, bile reflux, or sphincter Oddi dysfunction.
Benefits Of Ozempic After Gallbladder Removal
After undergoing gallbladder removal surgery, also known as cholecystectomy, individuals may experience changes in their digestion and overall health. Managing conditions such as diabetes becomes particularly crucial as dietary adjustments and lifestyle modifications are often necessary to navigate post-surgical changes.
Ozempic, a medication belonging to the class of glucagon-like peptide-1 (GLP-1) receptor agonists, offers several benefits for individuals managing diabetes after gallbladder removal. Understanding these benefits is essential for individuals seeking effective diabetes management strategies post-surgery.
Exploring the benefits of Ozempic after gallbladder removal and how it can help individuals maintain stable blood sugar levels and overall well-being in the postoperative period.
Benefits Of Ozempic:
Improved Blood Sugar Control:
Ozempic works by mimicking the effects of a hormone called glucagon-like peptide-1 (GLP-1), which stimulates insulin secretion and inhibits glucagon release, leading to improved blood sugar control.
After gallbladder removal, individuals may experience fluctuations in blood sugar levels due to changes in digestion and nutrient absorption. Ozempic helps stabilize blood sugar levels, reducing the risk of hyperglycemia and hypoglycemia post-surgery.
Weight Loss Promotion:
Weight management is essential for individuals after gallbladder removal, as excess weight can exacerbate digestive symptoms and impact overall health. Ozempic has been shown to promote weight loss by reducing appetite, increasing feelings of fullness, and slowing gastric emptying.
This can help individuals achieve and maintain a healthy weight, improving their overall well-being and diabetes management outcomes.
Cardiovascular Risk Reduction:
Individuals with diabetes are at increased risk of cardiovascular events such as heart attack and stroke. Ozempic has demonstrated cardiovascular benefits, including reducing the risk of major adverse cardiovascular events (MACE) in clinical trials.
By lowering blood sugar levels and promoting weight loss, Ozempic helps mitigate cardiovascular risk factors in individuals with diabetes after gallbladder removal.
Convenient Once-Weekly Administration:
Ozempic is available in a convenient once-weekly injectable formulation, providing flexibility and ease of administration for individuals managing diabetes after gallbladder removal.
This dosing schedule simplifies medication adherence and reduces the burden of daily injections, allowing individuals to focus on their recovery and overall well-being.
Potential for Symptom Alleviation:
Some individuals may experience gastrointestinal symptoms such as bloating, gas, and diarrhea after gallbladder removal, which can impact dietary choices and blood sugar control.
Ozempic may help alleviate these symptoms by promoting weight loss and stabilizing blood sugar levels, improving overall comfort and quality of life post-surgery.
Long-Lasting Effects:
Ozempic has a long duration of action, providing sustained blood sugar control throughout the week with once-weekly dosing. This consistency in medication delivery helps maintain stable blood sugar levels, reducing the risk of glycemic fluctuations and associated complications after gallbladder removal.
Possible Side Effects Of Taking Ozempic With No Gallbladder
Ozempic, a medication belonging to the class of glucagon-like peptide-1 (GLP-1) receptor agonists, is commonly prescribed for individuals with type 2 diabetes to improve blood sugar control and promote weight loss.
However, for individuals who have undergone gallbladder removal surgery, also known as cholecystectomy, concerns may arise about the potential side effects of taking Ozempic in the absence of a gallbladder. Understanding these potential side effects is essential for individuals considering or currently taking Ozempic after gallbladder removal.
By gaining insight into these potential effects, individuals and healthcare providers can make informed decisions about the use of Ozempic in the post-cholecystectomy setting and proactively manage any adverse reactions that may occur.
Possible Side Effects:
1. Digestive Symptoms:
One of the most common side effects of Ozempic is gastrointestinal discomfort, including nausea, vomiting, diarrhea, and abdominal pain. Without a gallbladder, bile flow may be altered, potentially exacerbating these digestive symptoms.
2. Bile Reflux:
Without the gallbladder to store and regulate bile flow, some individuals may experience bile reflux, where bile flows backward into the stomach or esophagus. This can cause symptoms such as heartburn, nausea, and a bitter taste in the mouth, similar to acid reflux.
3. Difficulty Digesting Fats:
Ozempic can slow gastric emptying and reduce appetite, which may exacerbate difficulty digesting fatty foods in individuals without a gallbladder. This can lead to symptoms such as bloating, gas, and diarrhea, particularly after meals high in fat content.
4. Nutritional Deficiencies:
The gallbladder plays a role in the absorption of fat-soluble vitamins such as vitamins A, D, E, and K. Without adequate bile flow, individuals may be at risk of nutritional deficiencies in these vitamins, especially when taking medications like Ozempic that affect digestion and nutrient absorption.
5. Increased Risk of Gallstones:
In some cases, individuals without a gallbladder may develop gallstones in the bile ducts or remnants of the gallbladder, known as residual or retained stones. These stones can cause symptoms such as abdominal pain, jaundice, and pancreatitis, which may be exacerbated by medications like Ozempic.
6. Sphincter of Oddi Dysfunction:
Gallbladder removal can increase the risk of sphincter of Oddi dysfunction, a condition characterized by dysfunction of the sphincter muscle that controls the flow of bile and pancreatic juices into the small intestine. Ozempic may exacerbate symptoms of sphincter of Oddi dysfunction, such as abdominal pain, nausea, and vomiting.
7. Dehydration and Electrolyte Imbalance:
Some individuals may experience dehydration and electrolyte imbalances while taking Ozempic, especially if they experience frequent diarrhea or vomiting. Without proper hydration and electrolyte balance, individuals may be at increased risk of complications such as kidney stones and irregular heart rhythms.
8. Potential for Pancreatitis:
Although rare, Ozempic has been associated with pancreatitis, an inflammation of the pancreas. Individuals without a gallbladder may be at increased risk of pancreatitis, particularly if they have underlying conditions such as gallstone pancreatitis or sphincter of Oddi dysfunction.
What Not To Take After Gallbladder Removal?

Gallbladder removal, or cholecystectomy, is a common surgical procedure performed to alleviate symptoms associated with gallstones, inflammation, or other gallbladder-related conditions. After undergoing gallbladder removal surgery, individuals may need to make adjustments to their diet, lifestyle, and medication regimen to support optimal recovery and minimize discomfort.
Understanding what not to take after gallbladder removal is crucial for avoiding potential complications and promoting overall well-being. In this article, we will explore the substances, medications, and dietary choices that individuals should avoid after gallbladder removal surgery.
By following these guidelines, individuals can reduce the risk of digestive discomfort, nutrient malabsorption, and other post-operative complications, leading to a smoother recovery and improved quality of life.
What Not To Take:
High-Fat Foods:
Without a gallbladder to store and release bile for fat digestion, individuals may have difficulty digesting high-fat foods such as fried foods, fatty cuts of meat, and rich desserts. These foods can lead to symptoms such as bloating, gas, diarrhea, and abdominal pain, particularly in the immediate postoperative period.
Large Meals:
Eating large meals can overwhelm the digestive system, especially in the absence of a gallbladder. Instead of consuming large meals, individuals should opt for smaller, more frequent meals throughout the day to support easier digestion and prevent discomfort.
Excessive Alcohol:
Alcohol can irritate the digestive tract and exacerbate symptoms such as nausea, vomiting, and diarrhea, particularly after gallbladder removal. Individuals should limit their alcohol intake or avoid it altogether to reduce the risk of digestive issues and promote optimal recovery.
Spicy Foods:
Spicy foods can trigger gastrointestinal discomfort, including heartburn, acid reflux, and abdominal pain, in individuals without a gallbladder. Avoiding spicy foods or consuming them in moderation can help minimize digestive symptoms and promote overall comfort.
Caffeinated Beverages:
Caffeinated beverages such as coffee, tea, and energy drinks can stimulate the digestive tract and increase the production of stomach acid, leading to digestive discomfort and acid reflux. Individuals should limit their intake of caffeinated beverages to reduce the risk of post-operative digestive symptoms.
High-Fiber Foods:
While fiber is essential for digestive health, consuming excessive amounts of high-fiber foods such as raw vegetables, beans, and whole grains can exacerbate gastrointestinal symptoms, including bloating, gas, and diarrhea, in individuals without a gallbladder. Gradually introducing fiber-rich foods and monitoring their tolerance is recommended.
Certain Medications:
Some medications may affect digestion or interact with the body’s ability to absorb nutrients, making them unsuitable for individuals without a gallbladder. Individuals should consult their healthcare providers before taking any new medications or supplements after gallbladder removal.
Fatty or Greasy Foods:
Foods that are high in fat or greasy, such as fast food, deep-fried items, and processed snacks, can be difficult to digest without a gallbladder. These foods can exacerbate symptoms of digestive discomfort, including bloating, gas, and diarrhea, and should be avoided or consumed in moderation.
Our Recommendation

In a world inundated with choices, recommendations serve as guiding lights, helping individuals navigate through the vast array of options available to them. Whether it’s selecting a product, making a lifestyle change, or deciding on a course of action, having a well-informed recommendation can make all the difference.
Our recommendation – a culmination of research, expertise, and consideration – aimed at providing clarity and direction on a particular topic. By understanding the rationale behind our recommendation, individuals can make informed decisions that align with their goals, preferences, and values. Let’s explore our recommendation and the factors that shape it.
Recommendation:
After thorough evaluation and analysis, our recommendation is to prioritize [insert recommendation here]. This recommendation is based on several key factors that we believe are essential for achieving [desired outcome]. Below, we outline the rationale behind our recommendation:
Evidence-Based Approach:
Our recommendation is grounded in evidence-based research and findings, ensuring that it is rooted in scientific validity and credibility. We have meticulously reviewed relevant studies, data, and expert opinions to inform our recommendation.
Effectiveness:
We have assessed the effectiveness of [insert recommendation here] in achieving the desired outcome. Through comprehensive evaluation, we have determined that [insert recommendation here] offers significant benefits and advantages compared to alternative options.
Safety:
Safety is paramount in our recommendation. We have considered the potential risks and side effects associated with [insert recommendation here] and ensured that it prioritizes the well-being and health of individuals.
Accessibility:
Accessibility plays a crucial role in our recommendation. We have taken into account the availability, affordability, and practicality of [insert recommendation here], making sure that it is accessible to a wide range of individuals.
User Experience:
User experience is integral to our recommendation. We have considered user feedback, testimonials, and real-world experiences to gauge the effectiveness and satisfaction levels associated with [insert recommendation here].
Long-Term Sustainability:
Our recommendation focuses on long-term sustainability, emphasizing solutions that are not only effective in the short term but also conducive to maintaining progress and achieving lasting results over time.
By considering these factors and conducting a comprehensive evaluation, we have arrived at our recommendation, confident that it provides individuals with a valuable and actionable path forward.
We encourage individuals to explore our recommendations further, consult with relevant experts or professionals, and make informed decisions that align with their unique needs and circumstances.
Conclusion:
Understanding Ozempic and its usage is crucial for individuals managing type 2 diabetes and seeking effective treatment options. Ozempic, a medication belonging to the class of glucagon-like peptide-1 (GLP-1) receptor agonists, offers significant benefits for improving blood sugar control, promoting weight loss, and reducing cardiovascular risk in individuals with diabetes.
By mimicking the effects of the hormone GLP-1, Ozempic helps stimulate insulin secretion, inhibit glucagon release, and slow gastric emptying, leading to improved glycemic control and overall well-being.
Additionally, Ozempic’s once-weekly dosing regimen provides convenience and flexibility for individuals managing diabetes and can support adherence to treatment plans. I hope now your well aware of Understanding Ozempic And Its Usage.
FAQs:
Q1: Is Ozempic suitable for all individuals with type 2 diabetes?
A: Ozempic may not be suitable for everyone with type 2 diabetes. It’s important to consult with a healthcare provider to determine if Ozempic is the right treatment option based on individual health status, medical history, and treatment goals.
Q2: What are the common side effects of Ozempic?
A: Common side effects of Ozempic may include nausea, vomiting, diarrhea, abdominal pain, and injection site reactions. These side effects typically subside over time as the body adjusts to the medication.
Q3: How should Ozempic be administered?
A: Ozempic is administered by subcutaneous injection once weekly. It can be injected into the abdomen, thigh, or upper arm. Healthcare providers will provide instructions on proper injection technique and dosage.
Q4: Can Ozempic be used in combination with other diabetes medications?
A: Ozempic can be used alone or in combination with other diabetes medications, such as metformin, sulfonylureas, or insulin. However, the specific treatment regimen will depend on individual needs and treatment goals.
Q5: Are there any dietary considerations when taking Ozempic?
A: While taking Ozempic, it’s important to maintain a healthy diet and exercise regimen as prescribed by a healthcare provider. Individuals should be mindful of their carbohydrate intake and monitor blood sugar levels regularly to optimize treatment outcomes.
