Oral cancer, a serious and potentially life-threatening condition, affects millions of people worldwide each year. While it can occur for various reasons, understanding the underlying causes is essential for prevention, early detection, and effective treatment.
From lifestyle choices to genetic predispositions, several factors contribute to the development of oral cancer. By delving into these causes, we can shed light on the importance of awareness, education, and proactive measures in combating this disease.
Let’s explore the multifaceted nature of oral cancer causation and uncover ways to reduce risk and promote oral health.
What Causes Oral Cancer
1. Tobacco Use:
Tobacco products, including cigarettes, cigars, and smokeless tobacco, contain carcinogenic substances that can damage the cells in the mouth and throat, leading to the development of oral cancer.
2. Excessive Alcohol Consumption:
Chronic and heavy alcohol consumption is strongly associated with an increased risk of oral cancer. Alcohol can irritate the lining of the mouth and throat, making it more susceptible to cancerous changes.
3. Human Papillomavirus (HPV) Infection:
Certain strains of the human papillomavirus (HPV), particularly HPV-16 and HPV-18, have been linked to the development of oral cancer. HPV-related oral cancers often occur in the back of the throat, including the base of the tongue and tonsils.
4. Sun Exposure:
Prolonged exposure to sunlight, particularly on the lips, can increase the risk of developing oral cancer. UV radiation from the sun can damage the DNA in lip cells, leading to abnormal cell growth and the formation of cancerous lesions.
5. Poor Oral Hygiene:
Neglecting oral hygiene practices, such as regular brushing, flossing, and dental check-ups, can contribute to the accumulation of bacteria, plaque, and other harmful substances in the mouth, increasing the risk of oral cancer.
6. Dietary Factors:
A diet low in fruits and vegetables and high in processed foods, red meat, and saturated fats has been associated with an increased risk of oral cancer. Conversely, a diet rich in fruits, vegetables, and whole grains may help reduce the risk.
7. Genetic Predisposition:
While lifestyle factors play a significant role in the development of oral cancer, genetic predisposition can also influence an individual’s susceptibility to the disease. Certain genetic mutations or inherited conditions may increase the risk of oral cancer.
8. Age and Gender:
Oral cancer is more common in older adults, particularly those over the age of 45. Men are also at a higher risk of developing oral cancer compared to women, although the gap is narrowing due to changes in smoking and drinking patterns.
What Is Oral Cancer

Oral cancer, a form of cancer that develops in the mouth or throat, is a significant health concern affecting millions of individuals worldwide. It encompasses cancers of the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and throat.
Oral cancer can be life-threatening if not diagnosed and treated early. While it can occur in anyone, certain factors such as tobacco use, excessive alcohol consumption, HPV infection, and sun exposure increase the risk.
Recognizing the signs and symptoms of oral cancer, as well as understanding its causes and risk factors, is crucial for early detection and effective treatment. In this article, we’ll delve into the complexities of oral cancer, explore its impact on oral health and overall well-being, and discuss preventive measures and treatment options available.
Exploring Oral Cancer: Understanding the Disease
Oral cancer refers to the abnormal growth of cells in the oral cavity or oropharynx, which includes the mouth and throat. It can manifest as a malignant tumor that invades surrounding tissues and may spread to other parts of the body if left untreated.
Oral cancer can affect various structures within the mouth and throat, including the lips, tongue, cheeks, gums, floor of the mouth, hard and soft palate, sinuses, and throat (pharynx). This type of cancer often begins as a small, painless lesion or sore in the mouth that doesn’t heal within a few weeks.
As it progresses, oral cancer may cause symptoms such as persistent mouth sores, red or white patches on the tongue or lining of the mouth, swelling or lumps in the mouth or neck, difficulty swallowing or chewing, hoarseness or persistent sore throat, and unexplained weight loss.
Several factors can increase the risk of developing oral cancer. These include tobacco use in any form (including smoking and smokeless tobacco), excessive alcohol consumption, infection with certain strains of the human papillomavirus (HPV), prolonged sun exposure to the lips, poor oral hygiene, a diet low in fruits and vegetables, genetic predisposition, and a weakened immune system.
Early detection of oral cancer is essential for successful treatment and improved outcomes. Dentists and oral health professionals play a crucial role in screening for oral cancer during routine dental check-ups. If suspicious lesions or abnormalities are detected, further diagnostic tests such as biopsies, imaging studies (such as X-rays or CT scans), and laboratory tests may be performed to confirm the diagnosis.
Treatment for oral cancer depends on factors such as the stage and location of the cancer, as well as the patient’s overall health and preferences. It may include surgery to remove the tumor, radiation therapy, chemotherapy, targeted therapy, or a combination of these approaches. Supportive care, such as nutritional counseling and speech therapy, may also be provided to help manage symptoms and improve quality of life.
Symptoms Of Oral Cancer

Oral cancer is a pervasive and potentially devastating disease that affects various structures within the mouth and throat. While it can manifest in different forms and locations, recognizing the symptoms of oral cancer is crucial for early detection and prompt treatment.
From persistent mouth sores to changes in oral tissues, these symptoms can often go unnoticed or be mistaken for less serious conditions. However, being aware of the signs and seeking medical attention if they persist is essential for improving outcomes and increasing survival rates.
Let’s explore the diverse array of symptoms associated with oral cancer, delve into their underlying causes, and discuss the importance of regular screenings and early intervention in combating this disease.
Understanding the Symptoms of Oral Cancer
Oral cancer can present with a variety of symptoms that may vary depending on the location and stage of the disease. Some of the most common signs and symptoms include:
1. Persistent Mouth Sores:
One of the hallmark symptoms of oral cancer is the presence of mouth sores that do not heal within a few weeks. These sores may be painless or may cause discomfort, making it difficult to eat, speak, or swallow.
2. Red or White Patches:
Red or white patches on the tongue, gums, or lining of the mouth are another common sign of oral cancer. These patches may be flat or slightly raised and may be accompanied by pain or irritation.
3. Swelling or Lumps:
Swelling, lumps, or thickening of oral tissues, including the lips, tongue, cheeks, or throat, can indicate the presence of oral cancer. These abnormalities may be palpable or visible and may cause pain or difficulty moving the mouth or jaw.
4. Difficulty Swallowing or Chewing:
Difficulty swallowing (dysphagia) or chewing (mastication) is a common symptom of oral cancer, particularly as the disease progresses. Patients may experience a sensation of food getting stuck in the throat or may have pain or discomfort while swallowing.
5. Hoarseness or Persistent Sore Throat:
Hoarseness, changes in voice quality, or a persistent sore throat that does not improve with time are potential signs of oral cancer, especially when accompanied by other symptoms such as difficulty swallowing or breathing.
6. Unexplained Weight Loss:
Unexplained weight loss, particularly when accompanied by other symptoms such as difficulty eating or swallowing, may indicate advanced oral cancer. Cancer cells can alter metabolism and lead to unintentional weight loss.
7. Ear Pain or Earache:
Ear pain or earache that is not related to an ear infection or other ear-related conditions may be a symptom of oral cancer, particularly when accompanied by other oral symptoms such as mouth sores or difficulty swallowing.
8. Changes in Dental Alignment:
Changes in dental alignment or bite, such as loose teeth, persistent jaw pain, or difficulty wearing dentures, can sometimes indicate the presence of oral cancer affecting the underlying bone or soft tissues. I hope after reading this far you understand about what causes oral cancer.
Oral Cancer Diagnosis

Oral cancer, a formidable adversary in the realm of oncology, poses significant challenges in its diagnosis and management. Prompt and accurate diagnosis is crucial for initiating timely treatment and improving patient outcomes.
However, diagnosing oral cancer can be complex due to its varied presentation and overlapping symptoms with other oral conditions.
From physical examinations to advanced imaging techniques and biopsy procedures, the diagnostic journey involves a comprehensive approach aimed at identifying and characterizing suspicious lesions or abnormalities.
In this article, we’ll delve into the intricacies of oral cancer diagnosis, explore the tools and techniques used by healthcare professionals, and discuss the importance of early detection in combating this disease.
Shedding Light On Oral Cancer Diagnosis
During the physical examination, healthcare professionals look for various signs and symptoms associated with oral cancer, such as persistent mouth sores, red or white patches on the tongue or lining of the mouth, swelling or lumps in the mouth or neck, difficulty swallowing or chewing, hoarseness or persistent sore throat, and unexplained weight loss.
In addition to the physical examination, diagnostic tests may be performed to further evaluate suspicious lesions or abnormalities. These tests may include:
• Biopsy:
A biopsy involves removing a small sample of tissue from the suspicious lesion or abnormal area in the mouth or throat. The tissue sample is then examined under a microscope by a pathologist to determine if cancer cells are present.
• Imaging Studies:
Imaging techniques such as X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans may be used to assess the extent of the cancer, identify metastasis (spread) to nearby lymph nodes or distant organs, and plan treatment.
• Endoscopy:
Endoscopy involves using a thin, flexible tube with a camera and light at the end (endoscope) to visually examine the inside of the mouth, throat, and upper digestive tract. This procedure allows healthcare professionals to assess the appearance of the oral tissues and obtain biopsies if necessary.
• Brush Biopsy or Cytology:
In some cases, a brush biopsy or cytology may be performed to collect cells from the surface of suspicious lesions or abnormalities. These cells are then examined under a microscope to look for signs of cancerous or precancerous changes.
Treatment For Oral Cancer

Facing a diagnosis of oral cancer can be daunting, but advances in medical technology and treatment options offer hope and a path forward for patients. Treatment for oral cancer is highly individualized, taking into account factors such as the stage of the cancer, its location, and the patient’s overall health and preferences.
From surgery to radiation therapy, chemotherapy, targeted therapy, and immunotherapy, various approaches may be used alone or in combination to combat this disease.
In this article, we’ll explore the diverse array of treatment options available for oral cancer, delve into their mechanisms of action, and discuss the importance of a multidisciplinary approach in achieving optimal outcomes for patients.
Navigating The Path To Healing:
Treating oral cancer often requires a comprehensive approach that combines multiple treatment modalities tailored to the individual needs of each patient. The primary goals of treatment are to remove the cancerous tissue, prevent its recurrence, and preserve function and quality of life.
The choice of treatment depends on several factors, including the stage and location of the cancer, as well as the patient’s overall health and preferences.
1. Surgery:
Surgery is a common treatment for oral cancer, particularly in early-stage disease. The goal of surgery is to remove the cancerous tumor and a margin of surrounding healthy tissue to ensure complete excision.
Depending on the size and location of the tumor, surgery may involve removing part or all of the affected tissue, as well as nearby lymph nodes if the cancer has spread.
2. Radiation Therapy:
Radiation therapy uses high-energy beams to target and destroy cancer cells. It may be used alone or in combination with surgery or chemotherapy, depending on the stage and location of the cancer.
Radiation therapy may be delivered externally (external beam radiation) or internally (brachytherapy) and can help shrink tumors, relieve symptoms, and reduce the risk of recurrence.
3. Chemotherapy:
Chemotherapy uses drugs to kill cancer cells or prevent them from growing and dividing. It may be used alone or in combination with surgery or radiation therapy, particularly in advanced or metastatic oral cancer. Chemotherapy drugs may be given orally or intravenously and can cause side effects such as nausea, hair loss, and fatigue.
4. Targeted Therapy:
Targeted therapy targets specific molecules or pathways involved in the growth and spread of cancer cells. It may be used in combination with other treatments, particularly for cancers that are resistant to traditional therapies. Targeted therapy drugs are often administered orally and can have fewer side effects than chemotherapy.
5. Immunotherapy:
Immunotherapy harnesses the body’s immune system to recognize and destroy cancer cells. It may be used alone or in combination with other treatments for certain types of oral cancer. Immunotherapy drugs, such as checkpoint inhibitors, work by blocking signals that cancer cells use to evade detection by the immune system.
6. Supportive Care:
In addition to cancer-directed treatments, supportive care plays a crucial role in managing symptoms and improving the quality of life for patients with oral cancer. This may include nutritional support, pain management, speech therapy, dental care, and psychosocial support to address emotional and practical concerns.
How Does Oral Cancer Affect My Body?
Oral cancer, a formidable adversary in the realm of oncology, not only poses a threat to oral health but can also have profound effects on the entire body. From the mouth and throat to distant organs and systems, the impact of oral cancer can be far-reaching and multifaceted.
Understanding how oral cancer affects the body is essential for patients, caregivers, and healthcare professionals alike.
In this article, we’ll explore the physiological and systemic effects of oral cancer, including its impact on oral function, nutrition, overall health, and quality of life.
By shedding light on the broader implications of this disease, we can better appreciate the importance of early detection, comprehensive treatment, and supportive care in mitigating its effects and improving outcomes for those affected by oral cancer.
Understanding The Impact:
Oral cancer can have a profound impact on various aspects of the body, both locally and systemically. Here’s how it can affect different areas and functions:
• Oral Function:
Oral cancer can impair essential functions such as chewing, swallowing, and speaking. Tumors or lesions in the mouth or throat may interfere with the movement of the tongue, lips, and jaw, making it difficult to eat, drink, or communicate effectively.
• Nutrition and Weight Loss:
Difficulty swallowing or chewing due to oral cancer can lead to nutritional deficiencies and unintended weight loss. Malnutrition and dehydration are common complications of oral cancer and its treatment, which can weaken the body and compromise immune function.
• Pain and Discomfort:
Oral cancer can cause pain, discomfort, or soreness in the mouth, throat, or jaw, making it challenging to eat, drink, or speak comfortably. Pain management strategies, including medications and supportive care, may be necessary to alleviate symptoms and improve quality of life.
• Speech and Communication:
Tumors or surgical interventions for oral cancer can affect speech and communication, leading to changes in voice quality, articulation, or fluency. Speech therapy may be helpful in restoring or improving communication skills for patients undergoing treatment for oral cancer.
• Psychological and Emotional Well-being:
The diagnosis and treatment of oral cancer can have profound psychological and emotional effects on patients and their families. Anxiety, depression, fear, and uncertainty are common reactions to the challenges posed by oral cancer, highlighting the importance of psychosocial support and counseling.
• Systemic Effects:
Oral cancer can metastasize (spread) to nearby lymph nodes, tissues, or organs, as well as distant sites in the body. Metastatic oral cancer can affect vital organs such as the lungs, liver, and bones, leading to serious complications and a poorer prognosis.
• Immune Function:
Cancer and its treatment can weaken the immune system, making patients more susceptible to infections and other illnesses. Maintaining immune function through proper nutrition, hydration, and supportive care is essential for optimizing outcomes and reducing the risk of complications.
• Overall Health and Quality of Life:
The cumulative effects of oral cancer on oral function, nutrition, psychological well-being, and systemic health can significantly impact the overall quality of life for patients.
Comprehensive treatment approaches that address these diverse aspects of care are essential for improving outcomes and enhancing the quality of life for individuals affected by oral cancer.
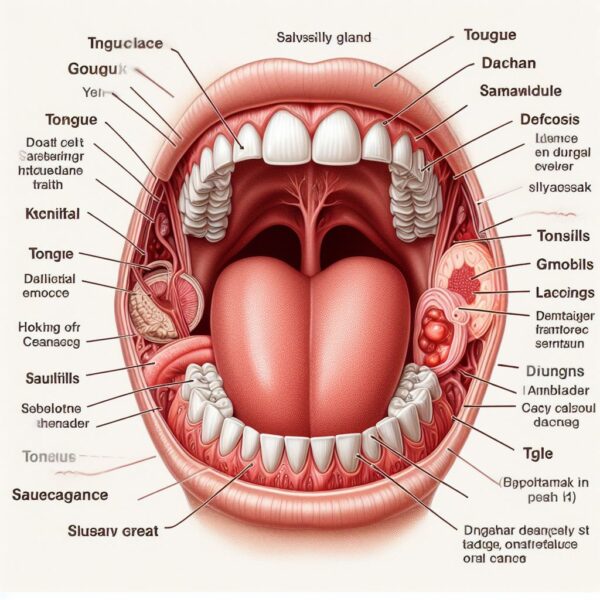
What Parts Of My Body Are In My Oral Cavity?
The oral cavity, often referred to as the mouth, is a complex and vital anatomical region that plays a central role in various essential functions, including eating, speaking, and breathing.
Comprising a diverse array of structures and tissues, the oral cavity serves as the gateway to the digestive and respiratory systems, facilitating the intake of food and air while also contributing to communication and sensory perception.
Understanding the components of the oral cavity and their interconnectedness is essential for maintaining oral health and overall well-being.
In this article, we’ll delve into the intricate anatomy of the oral cavity, explore its key components and functions, and highlight the importance of oral hygiene and regular dental care in preserving oral health and preventing disease.
Exploring The Components Of The Oral Cavity:
The oral cavity encompasses various structures that work together to perform essential functions related to digestion, respiration, and communication. Here’s an overview of the key components of the oral cavity:
• Lips and Cheeks:
The lips and cheeks form the outer boundaries of the oral cavity, providing support and protection to the inner structures. They contain muscles and glands that contribute to facial expression and saliva production.
• Teeth and Gums (Gingiva):
The teeth and gums are essential for chewing and breaking down food into smaller particles for digestion. Teeth are anchored within the jawbone by the periodontal ligament and surrounded by the gingiva, which helps protect the roots of the teeth and support their attachment to the bone.
• Tongue:
The tongue is a muscular organ located in the floor of the mouth that plays a crucial role in taste sensation, swallowing, and speech production. It contains taste buds that detect different flavors and textures, as well as muscles that facilitate movement and manipulation of food during chewing and swallowing.
• Palate:
The palate forms the roof of the mouth and is divided into two parts: the hard palate and the soft palate. The hard palate, located in the front portion of the mouth, is made up of bone and assists in the process of chewing and swallowing. The soft palate, located at the back of the mouth, helps close off the nasal passages during swallowing and speech to prevent food and fluids from entering the nose.
• Salivary Glands:
The salivary glands produce saliva, a watery fluid that helps moisten and lubricate the mouth, initiate the process of digestion, and protect the oral tissues from infection and injury. Major salivary glands include the parotid glands, submandibular glands, and sublingual glands, as well as numerous minor glands located throughout the oral cavity.
• Tonsils:
The tonsils are lymphoid tissues located at the back of the throat (oropharynx) that play a role in the immune system’s defense against infection. They help trap and filter out bacteria, viruses, and other foreign particles that enter the mouth and throat during breathing and swallowing.
• Floor of the Mouth:
The floor of the mouth is the area beneath the tongue and between the lower jawbone (mandible) and the tongue. It contains muscles, blood vessels, nerves, and salivary glands, as well as the openings of the submandibular and sublingual salivary ducts.
• Uvula:
The uvula is a small, fleshy projection located at the back of the soft palate. It plays a role in speech articulation and helps prevent food and fluids from entering the nasal passages during swallowing.
• Mucosa and Oral Mucous Membrane:
The mucosa and oral mucous membrane are specialized tissues that line the inner surfaces of the oral cavity, including the lips, cheeks, gums, tongue, palate, and floor of the mouth. They provide protection, sensation, and moisture to the oral tissues and play a role in immune defense.
Are There Oral Cancer Stages?
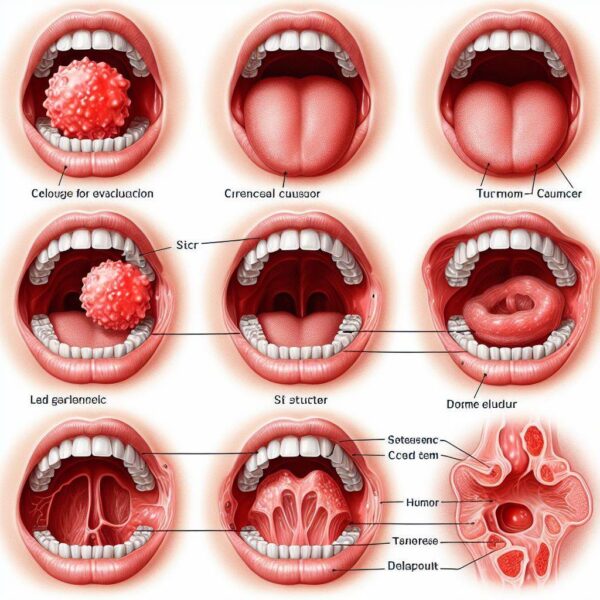
Oral cancer, like many other types of cancer, is characterized by a progression through various stages, each representing different degrees of severity and spread of the disease. These stages serve as a framework for healthcare professionals to assess the extent of the cancer, plan treatment strategies, and predict prognosis for patients.
Understanding the stages of oral cancer is crucial for patients and their families, as it provides valuable insight into the course of the disease and informs decisions regarding treatment options and supportive care.
In this article, we’ll explore the concept of oral cancer stages, delve into the criteria used to classify them and discuss the implications of staging on diagnosis, treatment, and prognosis.
Exploring Oral Cancer Stages:
1. Stage 0 (Carcinoma in situ):
In stage 0, also known as carcinoma in situ, abnormal cells are present in the lining of the oral cavity but have not invaded deeper tissues or spread to nearby lymph nodes or distant sites. At this stage, the cancer is confined to the surface layer of the mucosa and has not yet become invasive.
2. Stage I:
In stage I, the tumor is small (usually less than 2 centimeters in size) and limited to the oral cavity, without involvement of nearby lymph nodes or distant metastasis. Despite its small size, stage I oral cancer may still pose a significant risk if left untreated.
3. Stage II:
In stage II, the tumor may be larger (between 2 and 4 centimeters) and may have spread to nearby lymph nodes, but not to distant sites. The cancer remains confined to the oral cavity and has not yet invaded surrounding tissues or organs.
4. Stage III:
In stage III, the tumor is larger (greater than 4 centimeters) and may have invaded nearby tissues or structures, such as the tongue, jawbone, or throat. Lymph node involvement may also be present, either on the same side as the primary tumor or on both sides of the neck.
5. Stage IV:
Stage IV is the most advanced stage of oral cancer, characterized by a large tumor with extensive invasion of nearby tissues or structures, as well as spread to multiple lymph nodes or distant sites in the body.
Stage IV oral cancer may be further divided into subcategories (IVA, IVB, and IVC) based on the extent of tumor size, lymph node involvement, and metastasis.
Screening For Mouth Cancer
Mouth cancer, also known as oral cancer, is a serious and potentially life-threatening disease that affects thousands of individuals each year. Early detection is key to improving outcomes and increasing survival rates for patients with mouth cancer.
Screening for mouth cancer involves the systematic assessment of oral tissues and structures to identify any signs or symptoms of the disease at an early stage when treatment is most effective.
In this article, we’ll explore the importance of screening for mouth cancer, discuss the methods and techniques used in screening, and highlight the role of healthcare professionals and individuals in promoting early detection efforts.
Exploring Screening For Mouth Cancer:
Here’s a detailed look at the various aspects of screening for mouth cancer:
1. Risk Assessment:
Screening for mouth cancer often begins with a comprehensive risk assessment to identify individuals who may be at higher risk of developing the disease. Risk factors for mouth cancer include tobacco use (smoking and smokeless tobacco), excessive alcohol consumption, HPV infection, sun exposure to the lips, poor oral hygiene, and a history of oral cancer or precancerous lesions.
2. Visual Examination:
Visual examination of the oral cavity is a fundamental component of mouth cancer screening. Healthcare professionals, including dentists, oral surgeons, and primary care physicians, perform thorough examinations of the lips, gums, tongue, cheeks, palate, floor of the mouth, and throat to look for any abnormalities or suspicious lesions.
3. Physical Examination:
In addition to visual inspection, healthcare professionals may perform a physical examination of the oral cavity using specialized instruments and techniques. This may involve palpating (feeling) the oral tissues and lymph nodes to detect any lumps, swelling, or other abnormalities that may be indicative of mouth cancer.
4. Biopsy and Diagnostic Tests:
If suspicious lesions or abnormalities are identified during screening, further diagnostic tests such as biopsies, imaging studies (such as X-rays or CT scans), and laboratory tests may be performed to confirm the diagnosis of mouth cancer and assess the extent of the disease.
5. Self-Examination and Awareness:
Individuals can also play a role in screening for mouth cancer by performing regular self-examinations of their oral cavity and being aware of any changes or abnormalities that may arise. This includes checking for persistent mouth sores, red or white patches, lumps or swelling, difficulty swallowing or chewing, hoarseness, or unexplained weight loss.
6. Follow-Up and Monitoring:
Regular follow-up and monitoring are essential components of mouth cancer screening, particularly for individuals at higher risk of developing the disease. Healthcare professionals may recommend routine oral examinations and screening tests to detect any changes or recurrence of mouth cancer at an early stage.
Preventing Mouth Cancer
Mouth cancer, also known as oral cancer, poses a significant health threat worldwide, affecting millions of individuals each year. While certain risk factors for mouth cancer, such as tobacco use and excessive alcohol consumption, are well-established, there are proactive steps individuals can take to reduce their risk and promote oral health.
Prevention plays a critical role in combatting mouth cancer, emphasizing the importance of lifestyle modifications, regular dental care, and early detection efforts.
In this article, we’ll explore various strategies for preventing mouth cancer, delve into the role of risk factors and protective factors, and highlight the importance of education, awareness, and screening in reducing the burden of this disease.
Exploring Strategies For Preventing Mouth Cancer:
Preventing mouth cancer involves adopting a multifaceted approach that addresses both modifiable risk factors and protective factors associated with the disease. Here’s a detailed look at key strategies for preventing mouth cancer:
1. Tobacco Cessation:
Tobacco use, including smoking and smokeless tobacco products, is one of the most significant risk factors for mouth cancer. Quitting tobacco is the single most effective way to reduce the risk of developing mouth cancer and other tobacco-related diseases.
2. Limiting Alcohol Consumption:
Excessive alcohol consumption is another well-established risk factor for mouth cancer, particularly when combined with tobacco use. Limiting alcohol intake can help reduce the risk of developing the disease.
3. Healthy Diet and Nutrition:
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients and antioxidants that support overall health and reduce the risk of mouth cancer. Avoiding processed foods, sugary beverages, and excessive consumption of red and processed meats may also help lower the risk.
4. Sun Protection:
Sun exposure to the lips increases the risk of developing lip cancer. Using lip balms or sunscreen with SPF protection, wearing wide-brimmed hats, and seeking shade during peak sun hours can help protect the lips from harmful UV radiation.
5. HPV Vaccination:
Human papillomavirus (HPV) infection is a risk factor for certain types of mouth cancer, particularly in younger individuals. HPV vaccination can help prevent infection with high-risk HPV strains and reduce the risk of developing HPV-related mouth cancer.
6. Regular Dental Care:
Routine dental examinations and cleanings are essential for maintaining oral health and detecting any abnormalities or precancerous lesions early. Dentists can perform oral cancer screenings as part of regular check-ups and provide guidance on oral hygiene and lifestyle habits.
7. Oral Hygiene Practices:
Good oral hygiene, including brushing teeth twice a day, flossing daily, and using mouthwash, helps remove plaque, bacteria, and food debris from the mouth, reducing the risk of dental problems and gum disease that may contribute to mouth cancer.
8. Education and Awareness:
Educating individuals about the risk factors, signs, and symptoms of mouth cancer increases awareness and promotes early detection and intervention. Public health campaigns, community outreach programs, and patient education materials play a crucial role in raising awareness of mouth cancer prevention.
9. Regular Screening and Early Detection:
Routine oral cancer screenings, particularly for individuals at higher risk of developing the disease, can help detect any suspicious lesions or abnormalities early when treatment is most effective. Healthcare professionals, including dentists and primary care physicians, can perform screenings as part of regular check-ups.
Conclusion:
Understanding the factors that contribute to oral cancer is essential for promoting prevention, early detection, and effective treatment. While the exact causes of oral cancer may vary, several risk factors have been identified, including tobacco use, excessive alcohol consumption, HPV infection, sun exposure, poor oral hygiene, and a diet low in fruits and vegetables.
By addressing these risk factors through lifestyle modifications, vaccination, sun protection, and regular dental care, individuals can reduce their risk of developing oral cancer and improve their overall health and well-being.
Additionally, raising awareness of the signs and symptoms of oral cancer and promoting early detection efforts through routine screenings and education can further enhance outcomes for individuals affected by this disease. After reading so far you are fully aware of what causes oral cancer and how to keep yourself safe from it.
FAQs:
Q1: What are some common risk factors associated with oral cancer?
A: Common risk factors for oral cancer include tobacco use, excessive alcohol consumption, HPV infection, sun exposure to the lips, poor oral hygiene, and a diet low in fruits and vegetables.
Q2: How does tobacco use contribute to the development of oral cancer?
A: Tobacco use, including smoking and smokeless tobacco products, contains carcinogenic substances that can damage the cells lining the mouth and throat, increasing the risk of oral cancer.
Q3: Is HPV infection a risk factor for oral cancer?
A: Yes, certain strains of the human papillomavirus (HPV), particularly HPV-16 and HPV-18, have been linked to an increased risk of developing oral cancer, particularly in younger individuals.
Q4: Can excessive alcohol consumption increase the risk of oral cancer?
A: Yes, excessive alcohol consumption is a well-established risk factor for oral cancer, particularly when combined with tobacco use. Alcohol can irritate the oral tissues and increase the likelihood of cellular damage and cancer development.
Q5: How can individuals reduce their risk of developing oral cancer?
A: Individuals can reduce their risk of developing oral cancer by avoiding tobacco use, limiting alcohol consumption, practicing sun protection for the lips, maintaining good oral hygiene, eating a balanced diet rich in fruits and vegetables, and staying informed about the signs and symptoms of oral cancer for early detection and intervention.
